One way is through an insurance plan that is “supplemental” to the Medicare plan. For example, a treating LMFT may provide services to a patient who is a Medicare beneficiary and is also covered by a regular insurance plan (secondary to Medicare). The treating LMFT can bill the secondary insurance plan directly for the services rendered.
Full Answer
Are MFTs covered by Medicare?
In order for a mental health service to be covered by Medicare, the service must be for the diagnosis and treatment of mental illness. In addition, the mental health service must be delivered by a “covered” practitioner who is legally authorized to perform that service under state law. (MFTs are licensed in every state.)
Does Medicare cover MFTs under HR 945?
Sep 10, 2021 · Depending on the policy you select, you may only pay a deductible. The cost of family therapy, without Medicare, usually ranges between $75-$150 an hour. And, most therapists suggest one hour sessions each week for three months. Although, it really depends on your specific needs and care plan.
Does Medicare cover family therapy?
Medicare does not provide coverage for family or couple counseling if it is with a licensed Marriage and Family Therapist (MFT) unless they are employees of clinical facilities or are staff members at clinical offices of Medicare eligible practitioners. This is considered “incident two coverage” because a Medicare eligible practitioner must be present at the facility during …
Are marriage and family therapists eligible to participate in Medicare?
Background: In order for a mental health service to be covered by Medicare, the service must be for the diagnosis and treatment of mental illness. In addition, the mental health service must be delivered by a “covered” practitioner who is legally authorized to perform that service under state law. (MFTs are licensed in every state.)

How much does family therapy cost without Medicare?
Depending on the policy you select, you may only pay a deductible. The cost of family therapy, without Medicare, usually ranges between $75-$150 an hour. And, most therapists suggest one hour sessions each week for three months. Although, it really depends on your specific needs and care plan.
What are the medical professionals covered by Medicare?
If you get treatment from any of the following professionals, you have coverage: Clinical psychologist. Psychiatrist or doctor. Clinical social worker. Clinical nurse specialist. Nurse practitioner. Physician Assistant. Also, the facility where the service takes place must accept Medicare assignment.
What is part B in Medicare?
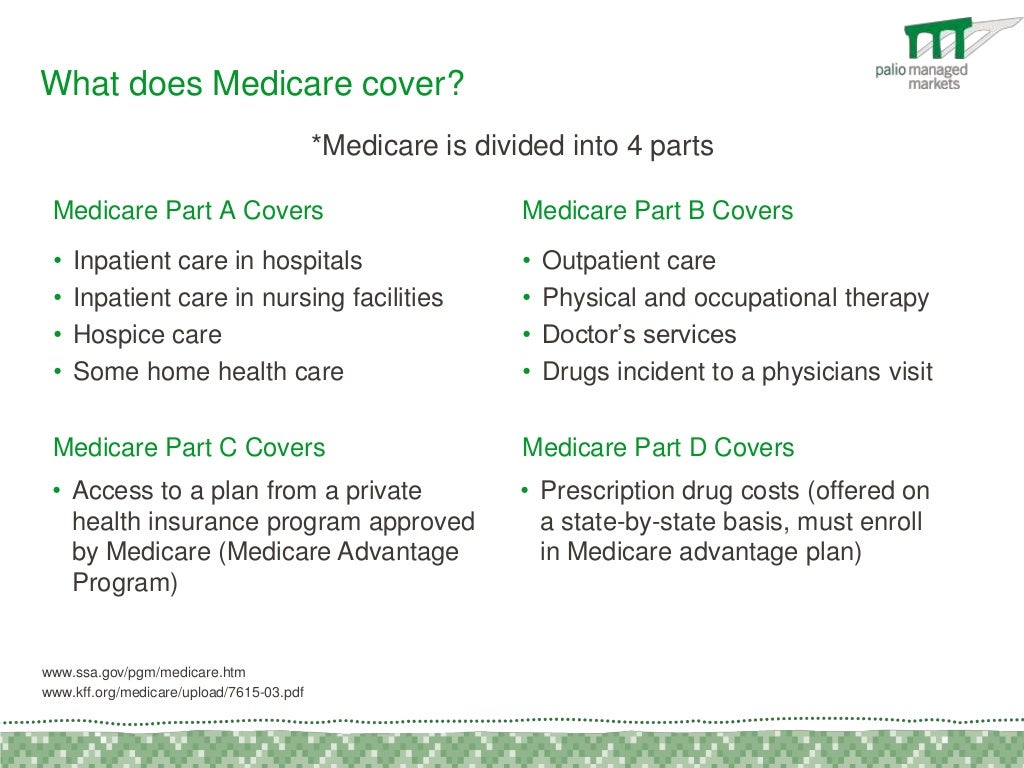
Part B covers family counseling. Family counseling includes marriage counseling. The purpose of the counseling must be to improve the patient’s mental health, and the provider must accept Medicare assignment. A professional must administer the counseling service to obtain coverage.
Does Medicare pay for mental health counseling?
Part B pays a portion of marital and family counseling costs to treat mental health. So, yes, Medicare will pay some of the costs. Now, you can sign up for a Medigap policy that would pick up the balance you’d otherwise pay. Depending on the policy you select, you may only pay a deductible.
Does Medicare cover outpatient mental health?
For Part B to cover the counseling, you must see a professional that accepts Medicare. Going to a doctor that doesn’t accept Medicare will mean you pay the full cost of care. Outpatient mental health services medicare covers include family therapy to help you through treatment.
Does Advantage Plan cover Part A?
Advantage plans must provide the same benefits as Part A and Part B. This means the Part B benefits that cover marital and family counseling are also available with an Advantage plan. If you’re on medication for depression, anxiety, or another mental health condition, an Advantage plan might also include Part D. Make sure to check the formulary to ensure it includes your prescriptions before signing up for a plan.
Does Medicare cover marriage counseling?
Marriage and family counseling can be helpful, but does Medicare cover this service? While these services are beneficial, Medicare will only cover under specific circumstances. For example, the service needs to be part of the treatment for mental illness.
What percentage of Medicare covers counseling?
Medicare Part B covers 80 percent of the cost of counseling therapy if it is provided by a behavioral health care provider such as a psychiatrist, physician, clinical psychologist, clinical social worker, or a nurse specialist.
What is family therapy?
Family therapy is a term that includes couples therapy, marriage counseling, and family systems therapy. It is a branch of psychotherapy meant for families and couples, or people in intimate relationships who need different types of behavioral health care.
What is marriage counseling?
Marriage counseling, couples therapy, or family therapy helps people in these relationships learn skills for building better, stronger bonds. They learn how to communicate openly, calmly and clearly, and how to solve problems rationally, without aggression or anger. Marriage counseling isn’t for everyone, but it may be just what you ...
What is the purpose of a therapist?
The goal of this form of therapy or counseling is to guide the partners in troubled relationships through difficult times and to help them develop and grow stronger. Therapists help couples find ways to improve communication, learn to resolve conflict without aggression or anger, and to address issues that are creating problems in the relationship.
How much does marriage counseling cost?
In the United States, the average hourly charge for marriage counseling, couples therapy, or family therapy from a professional equivalent to those covered through Medicare insurance, is between $75.00 and $150.00.
Does Medicare cover family counseling?
Medicare does not provide coverage for family or couple counseling if it is with a licensed Marriage and Family Therapist (MFT) unless they are employees of clinical facilities or are staff members at clinical offices of Medicare eligible practitioners.
How much does it cost to add MFTs to Medicare?
According to the Congressional Budget Office (CBO), the cost of adding both MFTs and licensed mental health counselors (LMHCs) to the Medicare program would total $100 million during its first five years, and $400 million during ten years (CBO Score: 111th HR 3962, Sec. 1308).
What is the role of MFTs in Medicare?
Federal government agencies also understand the valuable role MFTs play in increasing access to mental health services. The advisory committee to the Secretary of Health and Human Services recently encouraged inclusion of MFTs in the Medicare program.
What is the Mental Health Access Improvement Act of 2021?
Senate, the Mental Health Access Improvement Act of 2021 (HR 432 and S 828), that would add LMFTs, as well as LMHCs, as recognized Medicare providers. In 2020, the House Energy and Commerce Committee passed a prior version of this legislation (HR 945).
Does Medicare cover mental health?
In order for a mental health service to be covered by Medicare, the service must be for the diagnosis and treatment of mental illness. In addition, the mental health service must be delivered by a “covered” practitioner who is legally authorized to perform that service under state law. (MFTs are licensed in every state.)
Is a marriage and family therapist covered by Medicare?
Marriage and Family Therapists (MFTs) are not listed as Medicare-covered providers despite the fact that MFTs have education, training and practice rights equivalent to or greater than existing covered providers. Limited access to mental health services is a serious problem in the Medicare program.
What is Medicare preventive visit?
A one-time “Welcome to Medicare” preventive visit. This visit includes a review of your possible risk factors for depression. A yearly “Wellness” visit. Talk to your doctor or other health care provider about changes in your mental health. They can evaluate your changes year to year.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. applies. If you get your services in a hospital outpatient clinic or hospital outpatient department, you may have to pay an additional. copayment.
Can you do individual and group psychotherapy with a doctor?
Individual and group psychotherapy with doctors or certain other licensed professionals allowed by the state where you get the services.
Do you pay for depression screening?
You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is Medicare.org?
Comparing your Medicare options? Medicare.org ’s information and resources can help make it easy to find the quality and affordable Medicare plan that’s right for you. We offer free comparisons for Medicare Advantage Plans (Part C), Medicare Supplement Plans (Medigap), and Medicare Prescription Drug Plans (Part D).
What percentage of Medicare does a nurse practitioner pay?
Nurse practitioners. Physician assistants. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
Is counseling covered by Medicare?
Counseling and therapy are mental health services covered by Medicare Part B (Medical Insurance). This includes visits with the following health care providers who accept assignment:
Does Medicare cover mental health?
Medicare Coverage of Mental Health Services. A person’s mental health refers to their state of psychological, emotional, and social well-being – and it’s important to take care of it at every stage of life , from childhood to late adulthood. Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered ...
Does Medicare pay for depression screening?
Medicare Part B helps pay for one depression screening per year, and it must be done in a primary care doctor’s office or primary care clinic that can give follow-up treatment and referrals. In addition, Medicare beneficiaries are eligible to receive a one-time “Welcome to Medicare” preventive visit that includes a review of potential risk factors for depression.
Does Medicare cover grief and loss counseling?
Medicare Part B may help pay for family counseling if the goal of the therapy is related to helping your treatment. In addition, grief and loss counseling may be covered by Medicare for qualified hospice patients and their families, if it is provided by a Medicare-approved hospice and available in that state. Medicare does not cover other types of relationship counseling, such as marriage counseling. You’re only covered for mental health services from a licensed psychiatrist, clinical psychologist, or other health care professional who accepts Medicare assignment.
What are the extra benefits that Medicare doesn't cover?
Plans may offer some extra benefits that Original Medicare doesn’t cover—like vision, hearing, and dental services.
What happens if you don't get Medicare?
If you don't get Medicare drug coverage or Medigap when you're first eligible, you may have to pay more to get this coverage later. This could mean you’ll have a lifetime premium penalty for your Medicare drug coverage . Learn more about how Original Medicare works.
How much does Medicare pay for Part B?
For Part B-covered services, you usually pay 20% of the Medicare-approved amount after you meet your deductible. This is called your coinsurance. You pay a premium (monthly payment) for Part B. If you choose to join a Medicare drug plan (Part D), you’ll pay that premium separately.
What is Medicare Supplement Insurance?
You can get a Medicare Supplement Insurance (Medigap) policy to help pay your remaining out-of-pocket costs (like your 20% coinsurance). Or, you can use coverage from a former employer or union, or Medicaid.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is the original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). (Part A and Part B) or a.
Does Medicare Advantage cover prescriptions?
Most Medicare Advantage Plans offer prescription drug coverage. . Some people need to get additional coverage , like Medicare drug coverage or Medicare Supplement Insurance (Medigap). Use this information to help you compare your coverage options and decide what coverage is right for you.
How does LMFT work with Medicare?
Another way LMFTs may treat Medicare beneficiaries and obtain reimbursement is through “incident-to” billing. In some cases, however, Medicare will cover services by LMFTs if those services, although incidental, are considered an integral part of the services performed by physicians when treating their patients. In other words, a physician may submit claims for services rendered by an LMFT if those services are essential and fundamentally related to the services provided by the physician to the patient. These claims are reimbursed at 85 percent of the physician fee schedule. To bill “incident-to,” the physician must see new patients for an initial visit so that a physician-patient relationship can be established. Once the initial visit has occurred and the physician-patient relationship has been established, LMFT providers may render services to the patient during and after the initial visit, as long as the physician provides ongoing services to the patient that are of a frequency that demonstrate the physician’s active involvement in the patient’s care. There are other requirements that need to be met in order for physicians to bill for “incident-to” services by LMFTs. Those requirements are:
When did LMFTs become eligible for Medi-Cal?
On May 2, 2014, as a result of CAMFT’s advocacy efforts, LMFTs and Registered Interns were added to the list of eligible Medi-Cal providers per State Plan Amendment, SPA 14-012 (approved by the Centers for Medicare and Medicaid Services). This means LMFTs may enroll as Fee-For- Service providers directly with the State’s Medi-Cal system.
What is the number to call for Medi-Cal?
Providers, who have a question, need assistance or want to report a problem, may call 1-800-541-5555 to reach the Medi-Cal Provider Service Center.
How many people are covered by Medi-Cal?
Currently, approximately 13.5 million Californians are covered by Medi- Cal.
Is Medicare the same as Medi-Cal?
Given the similarities in the spelling of two large government programs, Medicare and Medi-Cal, there has been some confusion by providers. The programs, however, mainly serve different populations and have different rules about who is an eligible provider. This article offers an overview on how LMFTs and Registered Interns can provide services to Medi-Cal beneficiaries, the situations in which LMFTs can provide services to Medicare beneficiaries in California, and CAMFT’s recent advocacy efforts with respect to Medicare.
Can LMFTs provide services to Medicare beneficiaries?
This article offers an overview on how LMFTs and Registered Interns can provide services to Medi-Cal beneficiaries, the situations in which LMFTs can#N#provide services to Medicare beneficiaries in California, and CAMFT’s recent advocacy efforts with respect to Medicare.
Can LMFT be covered by Medicare?
For example, a treating LMFT may provide services to a patient who is a Medicare beneficiar y and is also covered by a regular insurance plan (secondary to Medicare). The treating LMFT can bill the secondary insurance plan directly for the services rendered.
What is the job of MFT?
The MFT’s job is to decipher the explicit and implicit messages communicated by a family up until the present moment. Knowing the homebrewed origin story of a person’s mental illness or disordered thinking and the relationships that have influenced it is key to being able to get at the heart of their distress.
What would an MFT do if a woman diagnosed with eating disorder decided to seek help for herself?
For example, if a woman diagnosed with an eating disorder decided to seek help for herself from a Marriage and Family Therapist, or an MTF, the MFT would sit with her and study her eating disorder in relation to her family experiences . What behaviors did this patient witness from her mom or dad that contributed to the development of this disorder? What unintended messages were communicated when granddad said she couldn’t leave the table until her dinner plate was clean? What did her aunt’s extensive makeup collection or her brother’s workout regime teach her about her body?
What is marriage and family therapy?
Marriage and Family Therapy is a specific branch of psychotherapy that examines the ways in which a family’s behaviors and dynamics impact its members. Sometimes it requires that an entire immediate family be involved in the treatment.
Is marriage and family therapy piecemeal?
Additionally, Medicaid coverage of Marriage and Family Therapy is piecemeal and continues to hamper the proper treatment of the nation’s most vulnerable populations.
When will the Mental Health Access Improvement Act of 2021 be passed?
And the ball has rolled! On January 21, 2021, the Mental Health Access Improvement Act of 2021, otherwise known as H.R. 432, was introduced to the House of Representatives. If passed, the bill will officially recognize and cover the essential services of mental health counselors and Marriage and Family Therapists under Medicare. ...
Does Medicare cover marriage and family therapy?
Why should Medicare and Medicaid cover Marriage and Family Therapy? As it stands, Marriage and Family Therapy is largely unrecognized by the federal government, making the services of MFTs unavailable to the low-income families, the elderly, and the disabled who lack the ability to pay for treatment out of pocket.