This information is pulled from NPPES, if the DOB or SSN is incorrect on the enrollment it cannot be update on the Medicare enrollment. The change must be done on paper. 3. The Individual Provider will select "Edit Name". 4. The user enters their new name and select "Next Page". The Provider's name mustbe updated on the NPI record in NPPES first.
How do I Change my Name or address with Medicare?
- Log in to my Social Security.
- Select the My Profile link on the right side of the screen.
- Select the Update Contact Information button and enter your address information.
- Select when would you like to schedule the update, then select Next.
- Review and verify your information, select Submit .
How to change a name on an approved Medicare enrollment?
Take the following additional actions to protect your Medicare enrollment information:
- Change your password in the I&A System before accessing PECOS the first time. ...
- Review your Medicare enrollment information several times a year to ensure no one altered information without your knowledge. ...
- Maintain your Medicare enrollment record. ...
- Store PECOS copies or paper enrollment applications in a secure location. ...
How do I Change my provider?
• It’s easy. Updating your settings takes only a few moments. How do I change my settings? Visit deltadentalins.com. Log in to your account. (If you don’t already have one, click Register Today to sign up.) 1. Turn the page to learn how to download Click on the My Profile tab. 2. Go to the Go Paperless section 3. Select Online and click Save.
How do I change my primary care doctor on Medicare?
- Network status. Choose a primary care provider that is in-network to save on out-of-pocket costs when you go to the doctor.
- Quality designations and board certifications. These show that the provider has taken extra steps to provide quality care.
- Location. Look for an office that's convenient to your home or work. ...
- Hospital affiliation. ...
How do I change my Pecos authorized official?
Steps for Setting Up Authorized Official & User in PECOSThe Authorized Official(s) of a Group is indicated on the Group's Medicare Enrollment application. ... https://pecos.cms.hhs.gov/pecos/login.do. ... Select View/Modify PECOS User Profile. ... Select Add Provider/Supplier Organization. ... Select Submit. ... USER SET-UP.More items...•
How do I add a new provider to Medicare?
Enrollment ApplicationsEnroll as a Medicare provider or supplier.Review information currently on file.Upload your supporting documents.Electronically sign and submit your information online.
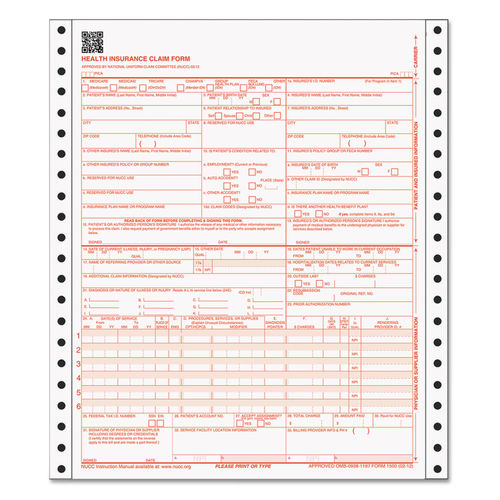
How do I fill out a CMS Form 855r?
3:579:18How to complete the CMS 855R Form to Reassign Medicare BenefitsYouTubeStart of suggested clipEnd of suggested clipSelect you are enrolling or currently enrolled in Medicare. And will be reassigning your benefitsMoreSelect you are enrolling or currently enrolled in Medicare. And will be reassigning your benefits indicate the effective date. And then complete all sections as instructed.
Is Pecos ID same as Medicare number?
The following walk-thru explains how a user can find their Medicare ID number in PECOS. Medicare numbers are also known as the CCN, P-Tan, Oscar, Provider number, or Medicare ID.
How long does it take to get a Medicare provider number?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health.
How do I fill out a CMS 460 form?
4:145:17Enrollment: CMS 460 Participation Agreement - YouTubeYouTubeStart of suggested clipEnd of suggested clipOrganizations at the bottom of the page have the authorized or delegated official signed date andMoreOrganizations at the bottom of the page have the authorized or delegated official signed date and list the office phone number this cannot be the contact person it must be an authorized or delegated.
What is the difference between 855I and 855R?
CMS-855I: For employed physician assistants (sections 1, 2, 3, 13, and 15). CMS-855R: Individuals reassigning (entire application). CMS-855O: All eligible physicians and non-physician practitioners (entire application). Same applications are required as those of new enrollees.
What is Medicare 855R?
Form CMS-855R is used by providers to reassign their right to bill the Medicare program and receive Medicare Part B payments to an eligible individual, clinic/group practice, or other health care organization.
How do I submit my Pecos 855R?
Providers and suppliers are able to submit their reassignment certifications either by signing section 6A and 6B of the paper CMS-855R application or, if completing the reassignment via Internet-based PECOS, by submitting signatures electronically or via downloaded paper certification statements (downloaded from www. ...
Is NPI the same as Medicare provider number?
Yes, you must have an NPI to do business with any health insurance company including Medicare. But, your NPI is NOT your Medicare provider number. You may obtain an NPI through NPPES by applying online, click here to go to their website. It's a quick and simple process.
What does Pecos ID mean?
PECOS stands for Provider, Enrollment, Chain, and Ownership System. It is the online Medicare enrollment management system that allows individuals and entities to enroll as Medicare providers or suppliers.
What is Pecos NPI?
PECOS stands for Provider Enrollment and Chain/Ownership System. NPI: First Name: Last Name: Search.
What is a private contract with Medicare?
This contract will reflect the agreement between you and your patients that they will pay out of pocket for services, and that nobody will submit the bill to Medicare for reimbursement.
What is PECOS Medicare?
PECOS is the online Medicare enrollment management system which allows you to: Enroll as a Medicare provider or supplier. Revalidate (renew) your enrollment. Withdraw from the Medicare program. Review and update your information. Report changes to your enrollment record. Electronically sign and submit your information.
How long does it take to withdraw from Medicare?
Withdraw from Medicare. If you retire, surrender your license, or no longer want to participate in the Medicare program, you must officially withdraw within 90 days. DMEPOS suppliers must withdraw within 30 days.
How often does an opt out affidavit renew?
If you’re currently opted out, your opt-out status will automatically renew every two years. If you submitted an opt-out affidavit before June 16, 2015 and never renewed it, you’ll need to submit a new opt-out affidavit.
Can you bill Medicare out of pocket?
You don’t want to bill Medicare for your services, but instead want your Medicare patients to pay out of pocket. Medicare coverage would apply when you order or certify items and services. If you choose to opt out of Medicare, you will not be able to bill for Medicare Advantage.
Updating your address or bank details
It’s quick and easy to update your address and bank details online. You can do this any time.
Updating your name, date of birth or gender
You can call us on the Medicare program line to make some updates to your name or date of birth. You’ll need to prove your identity over the phone.
Updating details when someone has died
If a family member listed on your card dies, you’ll need to let us know. On request, we can reissue a new card.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What is MLN CMS?
The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matters link.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.
Who should report changes in BCRC?
Beneficiary, spouse and/or family member changes in employment, reporting of an accident, illness, or injury, Federal program coverage changes, or any other insurance coverage information should be reported directly to the BCRC.
Does BCRC release beneficiary information?
You will be advised that the beneficiary's information is protected under the Privacy Act, and the BCRC will not release the information. The BCRC will only provide answers to general COB or MSP questions. For more information on the BCRC, click the Coordination of Benefits link.
How to change Medicare enrollment after getting an NPI?
Before applying, be sure you have the necessary enrollment information. Complete the actions using PECOS or the paper enrollment form.
How to get an NPI for Medicare?
Step 1: Get a National Provider Identifier (NPI) You must get an NPI before enrolling in the Medicare Program. Apply for an NPI in 1 of 3 ways: Online Application: Get an I&A System user account. Then apply in the National Plan and Provider Enumeration System (NPPES) for an NPI.
How to request hardship exception for Medicare?
You may request a hardship exception when submitting your Medicare enrollment application via either PECOS or CMS paper form. You must submit a written request with supporting documentation with your enrollment that describes the hardship and justifies an exception instead of paying the application fee.
What are the two types of NPIs?
There are 2 types of NPIs: Type 1 (individual) and Type 2 (organizational). Medicare allows only Type 1 NPIs for solely ordering items or certifying services. Apply for an NPI in 1 of 3 ways:
How long does it take to become a Medicare provider?
You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
What is Medicare Part B?
Medicare Part B claims use the term “ordering/certifying provider” (previously “ordering/referring provider”) to identify the professional who orders or certifies an item or service reported in a claim. The following are technically correct terms:
What is Medicare revocation?
A Medicare-imposed revocation of Medicare billing privileges. A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program. A conviction of a federal or state felony within the 10 years preceding enrollment, revalidation, or re-enrollment.