Medicare and Employer Insurance Coverage
- Individuals age 65 and over who currently receive group health plan coverage from their employers are also eligible for Medicare.
- Depending on the size of the company, these individuals may choose to enroll into Medicare immediately or delay enrollment until a later date.
- Medicare can be used along with a group health plan to cover most necessary medical services and needs.
Is Medicare better than employer insurance?
Their spouse can stay on their employer’s plan until they become eligible for Medicare, and though there are some exceptions, 65-year-old employees can benefit from both their employer’s plan and their Medicare plan. Contrary to popular belief, Medicare could actually provide better coverage at a lower cost than an employer plan.
Do you need Medicare if you have employer coverage?
Individuals age 65 and over who currently receive group health plan coverage from their employers are also eligible for Medicare. Depending on the size of the company, these individuals may choose to enroll into Medicare immediately or delay enrollment until a later date.
How does Medicare work with my current employer insurance?
- You will always have the choice of keeping your employer health insurance when you are eligible for Medicare if you work for a large company
- Depending on the size of your company, Medicare may be your primary or secondary insurance
- Medicare also works with COBRA, TRICARE, VA benefits, and HRAs
How does Medicare coordinate with employer health coverage?
- Who pays first for a car accident victim’s medical expenses? With coordinated benefits, health insurance is the primary payer. With uncoordinated benefits, No-Fault is the primary payer.
- Is coordinated coverage optional? Coordinated coverage of No-Fault and health insurance benefits is optional for drivers. ...
- Is one cheaper than the other? Yes. ...

Can you have employer coverage and Medicare at the same time?
Can I have Medicare and employer coverage at the same time? Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Is Medicare primary or secondary to employer coverage?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Can an employer contribute to Medicare premiums?
Can my employer pay my Medicare premiums? Employers can't pay employees' Medicare premiums directly. However, they can designate funds for workers to apply for health insurance coverage and premium payments with a Section 105 plan.
What is employer sponsored Medicare?
An employer (or union) retiree Medicare Advantage plan is a type of Medicare Advantage plan offered by a public or private employer or union. Retiree Medicare Advantage plans must follow Medicare rules, as required by the Center for Medicare & Medicaid Services (CMS).
Can I keep my private insurance and Medicare?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is a Section 105 plan?
A Section 105 Plan allows a qualified business owner to deduct 100% of. health insurance and dental insurance premiums for eligible employee(s) and family. This also includes qualified long-term care insurance. uninsured (out-of-pocket) medical, dental, and vision care expenses for eligible employee(s) and family.
How do I get reimbursed for Medicare premiums?
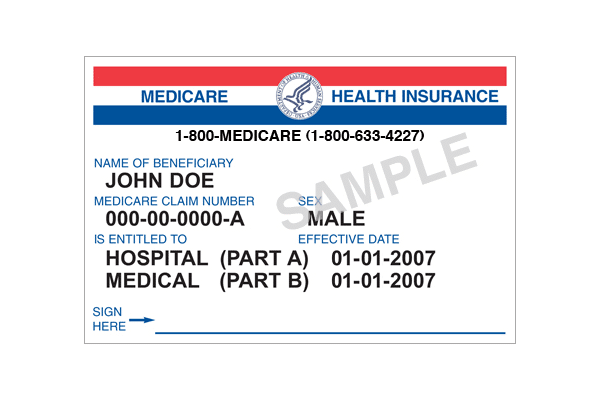
Call 1-800-MEDICARE (1-800-633-4227) if you think you may be owed a refund on a Medicare premium. Some Medicare Advantage (Medicare Part C) plans reimburse members for the Medicare Part B premium as one of the benefits of the plan. These plans are sometimes called Medicare buy back plans.
What is a Medicare Part B reimbursement?
The Medicare Part B Reimbursement program reimburses the cost of eligible retirees' Medicare Part B premiums using funds from the retiree's Sick Leave Bank. The Medicare Part B reimbursement payments are not taxable to the retiree.
What is the Medicare small employer exception?
If an employer, having fewer than 20 full and/or part-time employees, sponsors or contributes to a single-employer Group Health Plan (GHP), the Medicare Secondary Payer (MSP) rules applicable to individuals entitled to Medicare on the basis of age do not apply to such individuals.
Can I cancel Part B Medicare if I go back to work?
If you're going back to work and can get employer health coverage that is considered acceptable as primary coverage, you are allowed to drop Medicare and re-enroll again without penalties. If you drop Medicare and don't have creditable employer coverage, you'll face penalties when getting Medicare back.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
What is a small group health plan?
Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan. If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP).
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.
How old do you have to be to get Medicare?
Although retirement age usually ranges from 66 to 67 years old, Medicare eligibility for most individuals begins at age 65. Some people who continue to work past age 65 may also have group health plan benefits through their employer. Because of this, it’s possible to have both Medicare and a group health plan after age 65.
What is the number to call Medicare?
If you’re not sure whether Medicare will be the primary or secondary payer in your situation, you can call 855-798-2627 to speak to someone at Medicare’s Benefits Coordination & Recovery Center.
How to determine if Medicare is primary or secondary?
Here’s how to know who the primary and secondary payers are in your situation: 1 Medicare is generally the primary payer if the company you work for has fewer than 20 employees. But Medicare becomes the secondary payer if your employer is part of a group health plan with other employers who have more than 20 employees. 2 Medicare is typically the secondary payer if the company you work for has 20 or more employees. In this case, your group health plan is the primary payer and Medicare pays out only after your employer’s plan has paid their portion.
How long do you have to enroll in Medicare after you retire?
Once you retire and give up your employer health benefits, you will have a special enrollment period of 8 months to enroll in Part A and Part B, if you haven’t enrolled already. This special enrollment period begins the month after your employment or group health plan ends. There is no late enrollment penalty for enrolling in original Medicare ...
What is the primary payer?
When you receive medical services, your primary insurance pays out first. This insurance is known as the primary payer. If there’s anything that your primary insurance didn’t cover, your secondary insurance pays out next. This insurance is known as the secondary payer.
Does Medicare cover dependents?
Medicare is individual health insurance coverage, which means that it doesn’t include coverage for spouses or dependents. Most group health plans, on the other hand, do include some sort of coverage option for dependents and spouses.
Does Medicare work with employer benefits?
Instead, they can work in conjunction. Medicare is meant to work together with employer benefits to cover your healthcare needs and help pay for most, if not all, of your medical expenses.
What happens if you leave Medicare without a creditable coverage letter?
Without creditable coverage during the time you’ve been Medicare-eligible, you’ll incur late enrollment penalties. When you leave your group health coverage, the insurance carrier will mail you a creditable coverage letter. You’ll need to show this letter to Medicare to protect yourself from late penalties.
What is a Health Reimbursement Account?
Beneficiaries who participate can get tax-free reimbursements, including their Part B premium. A Health Reimbursement Account is a well-known Section 105 plan. An HRA reimburses eligible employees for their premiums, as well as other medical costs.
What happens if you don't have Part B insurance?
If you don’t, your employer’s group plan can refuse to pay your claims. Your insurance might cover claims even if you don’t have Part B, but we always recommend enrolling in Part B. Your carrier can change that at any time, with no warning, leaving you responsible for outpatient costs.
Is Medicare billed first or second?
If your employer has fewer than 20 employees, then Medicare becomes primary. This means Medicare is billed first, and your employer plan will be billed second. If you have small group insurance, it’s HIGHLY recommended that you enroll in both Parts A and B as soon as you’re eligible. If you don’t, your employer’s group plan can refuse ...
Is a $4,000 hospital deductible a creditable plan?
For your outpatient and medication insurance, a plan from an employer with over 20 employees is creditable coverage. This safeguards you from having to pay late enrollment penalties for Part B and Part D, ...
Is Part B premium free?
Since Part B is not premium-free like Part A is for most, you may wish to delay enrollment if you have group insurance. As stated above, the size of your employer determines whether your coverage will be considered creditable once you retire and are ready to enroll. Group coverage for employers with 20 or more employees is deemed creditable ...
Can employers contribute to Medicare premiums?
Medicare Premiums and Employer Contributions. Per CMS, it’s illegal for employers to contribute to Medica re premiums. The exception is employers who set up a 105 Reimbursement Plan for all employees. The reimbursement plan deducts money from the employees’ salaries to buy individual insurance policies.
Why is Medicare different from Cobra?
A Word About COBRA. Medicare coordinates differently with COBRA than it does with active coverage. This is important because so many people get this wrong and then owe penalties. When you are still actively working at a large employer, their Group Insurance pays primary and Medicare pays secondary.
When does Medicare change?
If that former employer DOES offer coverage, your benefits will likely change when you turn 65. This is because when you are age 65 and have retiree coverage, Medicare becomes your primary insurance, and your group coverage now pays secondary. Prices and benefits from your employer coverage may be different once you turn 65.
What is a 105 reimbursement plan?
A Section 105 Reimbursement Plan allows the employer to deduct expenses for employees who purchase individual health insurance plans. Eligible employees can participate and the employer can reimburse premiums for Medicare Parts A and B as well as Medigap plans.
How much is Medicare Part A deductible in 2021?
The Medicare Part A hospital deductible is $1,484 in 2021. So if you have both your employer insurance and Part A, and you incur a bill for a hospital stay, you will only be out $1,484 for your inpatient hospital services. Medicare pays the rest of any Part A services.
What does "active employer" mean?
Active employer coverage means you are still actively working, not retired. In this scenario, you have the right to remain on your employer’s group health insurance plan if you choose. Your Medicare benefits can coordinate with that coverage. HOW it coordinates depends on the size of your employer.
Does Medicare coordinate with employer insurance?
Medicare coordinates benefits with your employer coverage. You likely have options to keep your employer insurance and Medicare will coordinate with that coverage. You’ll also want to compare the cost of that employer coverage against what it would cost you to roll over to Medicare as your primary insurance.
Do you have to have Medicare if you are 65?
Medicare and Employer Coverage. If you are 65+ (or turning 65 soon) and will have both Medicare and Employer Coverage because you are still actively working, you will have a number of things to think through. Medicare coordinates benefits with your employer coverage. You likely have options to keep your employer insurance ...
If you're still working when you turn 65, you may be able to delay Medicare enrollment without penalty
If you're like many Americans getting ready to turn 65, you still have health insurance through an employer plan. However, just because you aren't ready to retire doesn't mean you aren't eligible for Medicare. In this post, we look at Medicare and employer coverage to help you understand your options and avoid late penalties.
How does Medicare coordinate with employer coverage?
The way Medicare coordinates with an employer insurance plan depends on the answers to two questions:
How Medicare works with an employer health plan
Medicare defines a large company as one that employs 20 or more people. If your group health plan is through a large employer, Medicare is your secondary payer. That means that Medicare pays after your employer plan pays its share.
Enrolling in Medicare when actively employed
If you are actively employed when you turn 65, Medicare enrollment is not automatic. That means you must sign up for Medicare through Social Security.
Keep your proof of creditable coverage
Having creditable coverage when you become eligible for Medicare qualifies you for a Special Enrollment Period (SEP). This means you can delay Medicare enrollment without incurring late penalties. However, you must be able to prove you had creditable coverage to qualify for the SEP.
What happens with Medicare if you go back to work after you retire?
Many Americans decide to go back to work after they retire. If this describes you, and your new job offers a group health plan, you may cancel Part B. Then, when you're ready to retire again, you'll qualify for another SEP. You'll also be able to enroll in a Medigap plan without having to undergo medical underwriting.
How Medicare works with COBRA
COBRA is a health insurance program that provides continued coverage for people who are no longer actively employed. The "actively employed" part is crucial. Remember, Medicare can only be secondary coverage if you are actively employed.
Who submits claims to Medicare?
Healthcare providers submit claims to the primary insurer first. Providers who participate with Medicare, which is known as accepting assignment, will usually send a claim directly to Medicare for consideration.
What are the rules for Medicare?
The coordination of benefits rules decide when Medicare pays first. They also ensure that: 1 the correct insurer pays claims 2 Medicare shares eligibility data with other health insurers, including employer insurance 3 claim payments do not exceed 100% of the total healthcare provider charges
Do I need to sign up for Medicare when I turn 65?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work.
How does Medicare work with my job-based health insurance?
Most people qualify to get Part A without paying a monthly premium. If you qualify, you can sign up for Part A coverage starting 3 months before you turn 65 and any time after you turn 65 — Part A coverage starts up to 6 months back from when you sign up or apply to get benefits from Social Security (or the Railroad Retirement Board).
Do I need to get Medicare drug coverage (Part D)?
You can get Medicare drug coverage once you sign up for either Part A or Part B. You can join a Medicare drug plan or Medicare Advantage Plan with drug coverage anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
