You’re generally eligible for Original Medicare (Part A and Part B) when you turn 65 or receive disability benefits, whether or not you’re married. If you’re married and haven’t worked in a paying job or didn’t work enough quarters, you may still qualify for premium-free Medicare Part A benefits through your spouse.
Full Answer
Do Your Medicare benefits cover your spouse?
Your personal Medicare insurance policy does not cover anyone but you. Your spouse or family members cannot be included in your coverage. For your spouse to have Medicare coverage, he or she must have a separate, individual policy.
Is spouse covered under Medicare?
Medicare will only cover you, not your spouse or children if they are not eligible on their own. This is where problems begin, especially when a working spouse is older than a non-working spouse. Say the working spouse turns 65, retires, and claims Medicare. The other spouse is only 61.
What is your Medicare spousal coverage?
- Age 65 or older
- Under age 65 with a qualifying disability
- Have End-Stage Renal Disease
How to apply online for retirement, spouses or Medicare benefits?
www.SocialSecurity.gov/benefits/retirement and select Apply for Retirement Benefits and then accept the terms of service to begin. SocialSecurity.gov Apply Online for Benefits Select one: • Start a New Application • Return to Saved Application Process Create or log in to your my Social Security account You need to log in to your my
Can someone have Medicare and private insurance at the same time?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
Do both spouses pay Medicare Part B premiums?
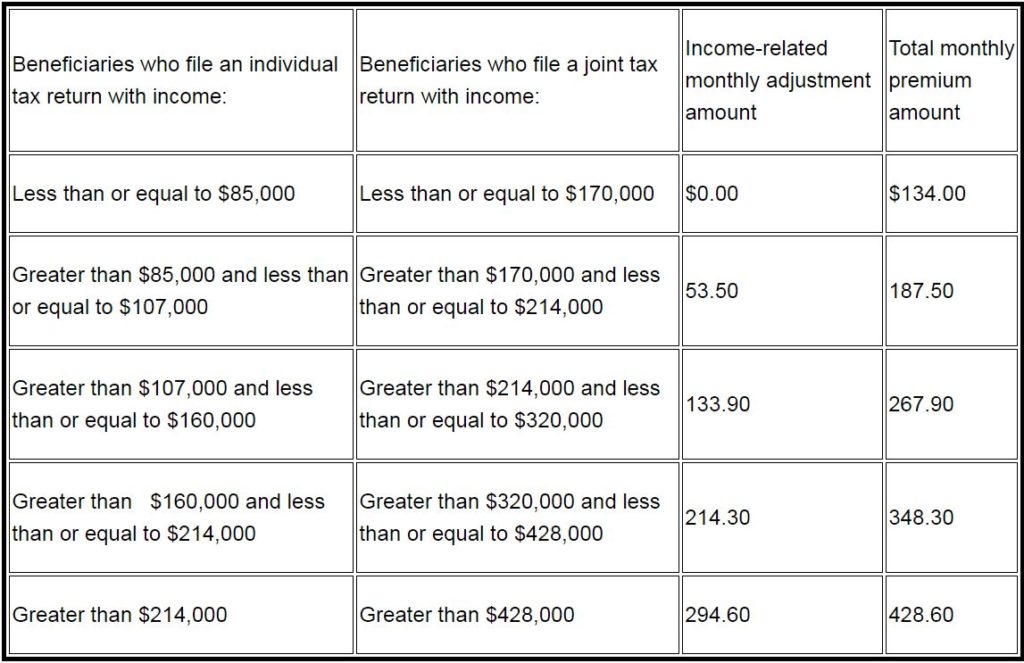
Medicare Part B Medicare considers you and your spouse's combined income (if you're married and file your income taxes jointly) when calculating Part B premiums. In most cases, you'll each pay the standard monthly Part B premium, which is $170.10 per month in 2022.
Can you have both Part A and Part B Medicare?
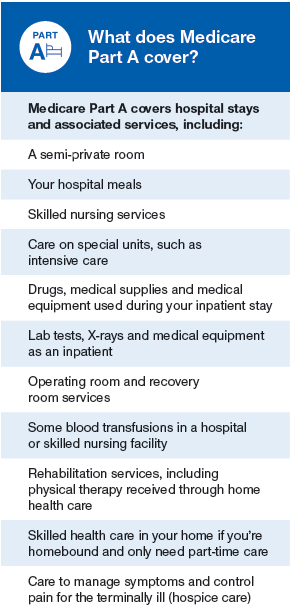
However, if you want to buy Medicare coverage and you want Part A, you also have to buy Part B. If you buy Part A and/or Part B (you must pay a premium for both), you must sign up during your Initial Enrollment Period, during a General Enrollment Period, or a Special Enrollment Period (see pages 11–13).
Do I need to enroll in Medicare Part B if my spouse is still working?
Generally, if you have job-based health insurance through your (or your spouse's) current job, you don't have to sign up for Medicare while you (or your spouse) are still working. You can wait to sign up until you (or your spouse) stop working or you lose your health insurance (whichever comes first).
Why is my Medicare Part B premium higher than my husbands?
Any changes in your Part B premiums are not related to your income but to your individual Social Security benefits. Any changes in your Part B premiums are not related to your income but to your individual Social Security benefits.
Can a husband and wife be on the same Medicare Advantage plan?
Medicare Advantage: what about my spouse? Medicare Advantage plans don't cover both you and your spouse together under one policy. Just as Medicare Part A and Part B cover each Medicare beneficiary separately, you can't share a Medicare Advantage plan with your spouse.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
Does secondary insurance cover primary deductible?
Does secondary insurance cover the primary deductible? Typically not. If you have a deductible on one or both plans, you will need to pay those deductibles before your insurance reimburses you for care.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Do you have to enroll in Medicare Part B every year?
Do You Need to Renew Medicare Part B every year? As long as you pay the Medicare Part B medical insurance premiums, you'll continue to have the coverage. The premium is subtracted monthly from most people's Social Security payments. If you don't get Social Security, you'll get a bill.
How do I delay Medicare Part B?
You may delay Part B and postpone paying the premium if you have other creditable coverage. You'll be able to sign up for Part B later without penalty, as long as you do it within eight months after your other coverage ends.
Is my spouse eligible for Medicare when I turn 65?
Your spouse is eligible for Medicare when he or she turns 65. Your eligibility for Medicare has no impact on the date that your spouse is eligible for Medicare. Continue reading for more answers to your questions about Medicare, individual health insurance, and coverage options for your spouse after you enroll.
How old do you have to be to get Medicare?
In a case such as this, you must be at least 62 years old.
How long do you have to work to qualify for Medicare?
In the United States, as soon as you turn 65 you are eligible for Medicare benefits if you are citizen or have been a legal resident for five years or more and have worked for at least 40 quarters (10 years) paying federal taxes.
Can you get Medicare at different ages?
If you and your spouse are different ages, you will likely become eligible at different times. Primary Medicare recipients and their non-insured spouses are entitled to the same benefits under Medicare if both have reached the age of 65.
Do you have to enroll in Medicare Part B or D?
If you wish to sign up for Medicare Part B (Medical Insurance), and/or Part D (prescription drug insurance), you must enroll separately during your initial enrollment period, Open Enrollment or during Special Enrollment Period to avoid paying late enrollment penalties.
Enrolling in Medicare at 65
If you want to enroll when you are turning 65, you can enroll in Medicare Parts A & B, Part D prescription drug coverage or a Medicare Advantage (Part C) plan. You can also look at adding a Medicare supplement insurance plan to Original Medicare (Parts A & B) to help with the out-of-pocket costs of Medicare.
Enrolling in Medicare Part A at 65
Many people who are covered by a spouse’s employer plan choose to either wait to enroll until they lose their spouse’s employer coverage or choose to only enroll in Part A since Part A usually has no premium.
Delaying Medicare Enrollment
Just because you are turning 65, doesn’t necessarily mean you have to get Medicare right now. If you decide that waiting to enroll in Medicare is the best option both financially and in terms of healthcare coverage for you, just follow Medicare’s rules, and you’ll avoid enrollment penalties when you do enroll.
When Would I Enroll If I Delay or Only Take Part A?
If you are able to delay enrolling in either all or part of Medicare, you will have a Special Enrollment Period of eight months that begins when the employer coverage is lost or when your spouse retires. During this time, you’ll be able to enroll in Medicare Parts A & B. You can also enroll in a Part D prescription drug plan.
Medicare Made Clear
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Medicare Made Clear
Whether you're just starting out with Medicare, need to brush up on the facts, or are helping a loved one, start your journey here.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens if you delay Medicare benefits?
By delaying Medicare benefits, you won’t have a primary insurer, and what you pay out-of-pocket will be high. In companies with more than 20 employees: Your employer becomes the primary insurer, with Medicare coverage second.
When does group insurance change?
Sometimes Group Insurance Changes When You Become Eligible for Medicare. Even if you know that your employer will be the primary insurer, take a look at your benefits. Sometimes they change when you become eligible for Medicare. Read over your group coverage benefits to see how they work once you or your spouse turn 65.
