Full Answer
How to Bill Tricare?
Telemedicine Billing Tips
- Synchronous Telemedicine Services. Synchronous telemedicine services involve an interactive, electronic information exchange in at least two directions in the same time period.
- Asynchronous Telemedicine Services. ...
- Billing FAQs. ...
What is Tricare allowable charge?
- The actual billed charge;
- The prevailing charge (or amount derived from a conversion factor) made for a given procedure, adjusted to reflect local economic conditions; or
- The maximum allowable charge.
Is Tricare considered health insurance?
Tricare is the health insurance plan for military members, their families, and retirees. There are many different types of Tricare available depending on your status and location: Tricare for Active Duty Members & Dependents. Retiree Tricare.
What are my Tricare for life costs?
• A yearly deductible before TRICARE cost-sharing will begin: $300 per individual/$600 per family. • For services beyond this deductible, you pay 50% of the TRICARE-allowable charge. • These costs do not apply to the catastrophic cap. TRICARE SELECT® (JAN. 1–DEC. 31, 2022) Includes TRICARE Select, TRICARE Overseas Program
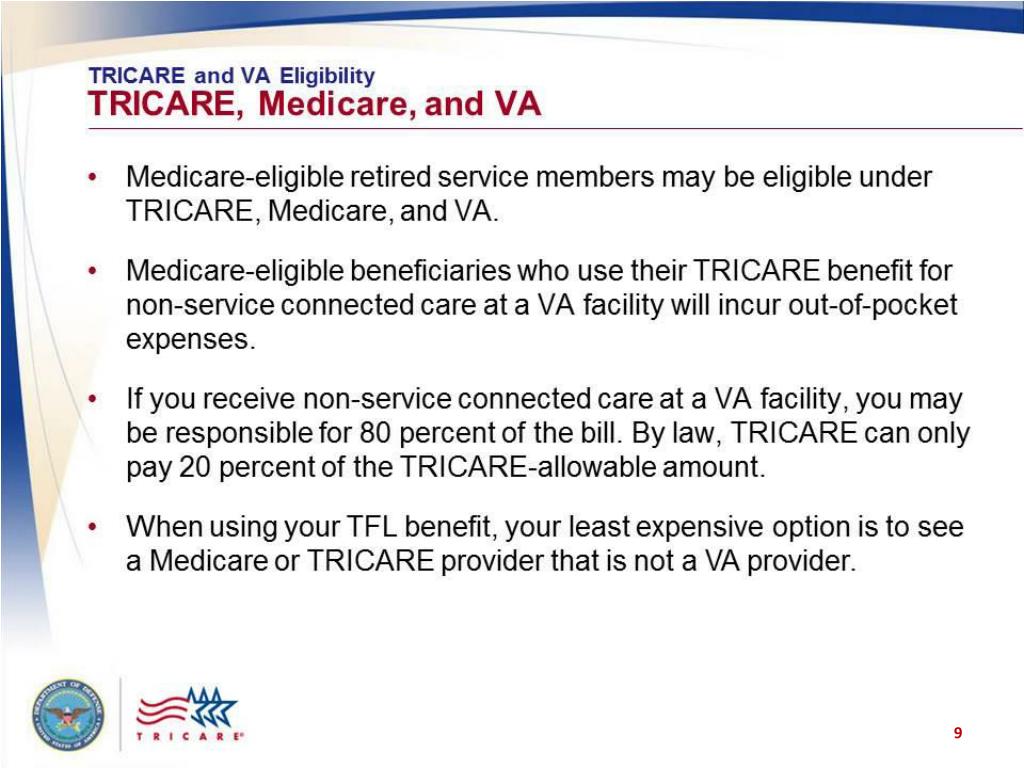
How Much Does TRICARE pay after Medicare?
“Since Medicare is the primary payer, it pays first—usually 80 percent of the Medicare allowable amount. TRICARE will then cover the remaining patient liability, provided the services you receive are a benefit of the TRICARE program.”
What percentage is Medicare reimbursement?
roughly 80 percentAccording to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
How does TRICARE coordinate with Medicare?
When you have Medicare Parts A and B, you automatically receive coverage fromTRICARE For Life. There are no enrollment forms or enrollment fees for TRICARE For Life. Medicare is your primary payer. TRICARE pays second to Medicare or last if you have other health insurance.
Does TRICARE follow Medicare rates?
TRICARE-eligible beneficiaries who have both Medicare Part A and B can use TRICARE For Life.
How much is the Medicare reimbursement for 2021?
If you are a new Medicare Part B enrollee in 2021, you will be reimbursed the standard monthly premium of $148.50 and do not need to provide additional documentation.
What is the Medicare conversion factor?
Basically, the relative value of a procedure multiplied by the number of dollars per Relative Value Unit (RVU) is the fee paid by Medicare for the procedure (RVUW = physician work, RVUPE = practice expense, RVUMP = malpractice). The Conversion Factor (CF) is the number of dollars assigned to an RVU.
What is the best Medicare plan for military retirees?
Military retirees with TRICARE For Life coverage may consider the AARP Medicare Advantage Patriot Plan. This plan provides the freedom to visit doctors and hospitals in our network for a $0 monthly premium and additional benefits that may include: Monthly credits applied to your Medicare Part B premium.
What happens to TRICARE when you turn 65?
TRICARE and Medicare beneficiaries who are age 65 must have Medicare Part A and Part B to remain TRICARE-eligible and be able to use TFL. TRICARE beneficiaries who aren't eligible for premium-free Medicare Part A at age 65 on their own work history or their spouse's work history remain eligible to enroll in USFHP.
Is TRICARE for Life free for military retirees?
Is TRICARE For Life free for military retirees? There are no enrollment fees or monthly premiums for retirees who are TRICARE beneficiaries. However, you must have Medicare Part A and B to qualify, and you have to pay Part B premiums, which are based on your income.
Do military retirees pay for Medicare Part B?
Military health coverage entitles the service person to delay Medicare Part B enrollment until a future date. They will be eligible for a Special Enrollment Period (SEP) to enroll in Medicare Part B without penalty when they leave active duty medical coverage.
Does TRICARE cover what Medicare doesn t?
Does TRICARE For Life cover the Medicare Part B deductible? If you're on active duty, your TRICARE coverage pays out first for your services covered under Medicare. If you have both TRICARE and Medicare, TRICARE pays the Medicare deductible and other services not covered by Medicare.
Do veterans pay for Medicare Part B?
Therefore, it is beneficial to enroll in the hospital insurance you earned through Medicare. However, like other beneficiaries, veterans with VA benefits will need to pay a standard Medicare Part B premium for Medicare's outpatient coverage. You will want to enroll in Medicare Part B as soon as you are eligible.
How much is a deductible for tricare?
The deductibles are $300 per individual/$600 per family. For services beyond this deductible, you pay 50% of the TRICARE-allowable charge. These costs don't apply to your catastrophic cap. Travel expensesAmounts you pay when traveling to and from your appointment.
What is a tricare authorized provider?
The fees you pay when you see a TRICARE-authorized providerAn authorized provider is any individual, institution/organization, or supplier that is licensed by a state, accredited by national organization, or meets other standards of the medical community, and is certified to provide benefits under TRICARE.
Does TRICARE cover EKG?
So if your doctor runs blood work as part of your visit, or you have an EKG or other test covered by TRICARE, you normally won't have a separate copayment for those tests.
Does tricare apply to active duty?
All TRICARE Plans. (Doesn't apply to active duty service members) Since some plans have cost-shares that are a percentage of the charge, a lower rate helps keep your costs down. That’s why it's usually less expensive for you to use a network provider for your care. Point-of-service fees.
Can you have more than one cost share for tricare?
All TRICARE Plans. (Doesn't apply to active duty service members) If you see several doctors as part of an appointment, or have additional tests, you may have more than one cost-share. For instance, if you have a surgery, you may have separate cost-shares for the facility, the surgeon, and the anesthesiologist.
Does Tricare reimburse for travel?
This includes costs for gas, meals, tolls, parking, lodging, local transportation, and tickets for public transportation. In some instances, TRICARE may reimburse your travel expenses for care. You can’t be on active duty.
What age does a retired person get tricare?
When retired service members or eligible family members reach age 65 and are eligible for Medicare, they become eligible for TRICARE For Life and are no longer able to enroll in other TRICARE plans.
How old do you have to be to get tricare?
Age 65 or older. Under age 65 with certain disabilities. ( If you have Medicare due to a disability, you can continue your TRICARE Prime enrollment [if you qualify]. If you do, your Prime enrollment fees are waived. You can also get a refund for any Prime enrollment fees that you paid.
What is Medicare Advantage?
Medicare Advantage (Medicare Part C) When using Original Medicare you may get health care services from any Medicare participating or Medicare Non-participating provider, regardless of their specialty. Medicare Part A is hospital insurance Which is financed by payroll deductions when you are or were working.
Does tricare waive enrollment fee?
TRICARE Prime will waive your individual enrollment fee. Please note: If you have TRICARE Prime or receive coverage from TRICARE For Life, your claims won’t process through the regional contractor. Providers file claims with Medicare first. Medicare processes and pays their portion of your claims.
Do you have to have Medicare Part B to get tricare?
If you have Medicare Part A, you must also have Medicare Part B to remain eligible for TRICARE, including prescription drug coverage. Your TRICARE coverage options when entitled to Medicare depend on your age:
Does Medigap pay out of pocket?
You pay a premium each month. Medigap pays your out-of-pocket costs in Original Medicare. If you’re eligible for TRICARE and have Medicare Part A and Part B, TRICARE For Life provides wraparound coverage which pays your out-of-pocket costs in Original Medicare for TRICARE covered services.
Do you need a break in coverage for tricare?
You can continue to get prescriptions filled with no break in coverage as long as you have Medicare Part B when you first become eligible for Medicare Part A. Medicare Part D, a prescription drug plan, is available to everyone with Medicare. You don't need Part D to keep TRICARE.
What is tricare medical?
Published by: Medicare Made Clear. TRICARE® is the health care program that serves uniformed service members, retirees and their families worldwide. Medicare is a federal health care program for U.S. citizens age 65 and older, under age 65 with certain disabilities and those who have end-stage renal disease. You may be eligible for both TRICARE and ...
How long do you have to enroll in tricare?
This means for Medicare, you’ll need to enroll during your Medicare Initial Enrollment Period. And with TRICARE, you have 90 days after you become eligible for Medicare to change your TRICARE health plan, and your plan options will depend on your specific situation including how you qualify for Medicare, you or a family member’s active duty status ...
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Is tricare for life a creditable benefit?
This allows you to sign up without paying the Part D late enrollment penalty. When you have TRICARE For Life and Medicare, you won’t receive a TRICARE wallet card.
Does Tricare work with Medicare?
TRICARE For Life may work with Original Medicare (Parts A & B), a Medicare Advantage plan or a Part D prescription drug plan. However, you may want to think carefully about whether you need Medicare drug coverage. TRICARE For Life includes a prescription drug benefit, so you may not need Part D.
Is tricare for life required?
TRICARE For Life is available worldwide and enrollment is not required. It offers secondary coverage after Medicare in the U.S. and U.S. Territories. In other overseas locations, TRICARE For Life is the primary payer.
Is there a fee for tricare for life?
Coverage is automatic if you have Parts A and B and pay your Part B premiums. There is no fee for enrolling in TRICARE For Life.
How much will tricare increase ASC?
Under the method discussed in this proposed rule, TRICARE's ASC payments would increase to certain providers by approximately $14 million. This is due to an increase in payments for surgical services that are paid under TRICARE's current ASC reimbursement methodology of approximately $23 million, with a decrease in payments for surgical services that are currently reimbursed outside TRICARE's current ASC reimbursement system of approximately $9 million. The overall impact represents an approximate 25-percent increase to ASCs for surgical services. For many procedures, the reimbursement amounts will increase by more than 25 percent. However, these increases will be offset by the fact that some procedures and devices that are currently paid separately will be bundled under this proposed reimbursement system.
What is the purpose of the tricare rule?
The purpose of this rule is to propose TRICARE regulation modifications necessary to implement for Ambulatory Surgery Centers (ASC) and Cancer and Children's Hospitals (CCHs) the statutory requirement that payments for TRICARE institutional services “shall be determined to the extent practicable in accordance with the same reimbursement rules as apply to payments to providers of services of the same type under [Medicare].” Although Medicare's reimbursement methods for ASC and CCHs are different, it is prudent to propose adopting both the Medicare ASC system and to adopt the Outpatient Prospective Payment System (OPPS) with hold-harmless adjustments (meaning the provider is not reimbursed less than their costs) for CCHs simultaneously to align with our statutory requirement to reimburse like Medicare at the same time. This rule sets forth the proposed regulatory modifications necessary to implement TRICARE reimbursement methodologies similar to those applicable to Medicare beneficiaries for outpatient services rendered in ASCs and cancer and children's hospitals.
What is an ASC in tricare?
Medicare defines an ASC as, “a distinct entity that operates exclusively for the purpose of furnishing outpatient surgical services to patients”; in this action we propose to adopt a definition at 32 CFR 199.2 that defines ASCs as those that meet the definition of an ASC under 42 CFR 416.2, including the requirement that they must participate in by Medicare as ASCs per 42 CFR 416.25, with exceptions for ASCs that do not have an agreement with Medicare due to the specialty populations they serve. Medicare also requires the provider to have an agreement with CMS; we propose that in lieu of separate certification by TRICARE, the ASC simply provide evidence that there is a valid agreement with Medicare. While the terms of the agreement with Medicare will not apply to TRICARE, only those providers with an agreement with Medicare (or those providers that meet certain exceptions as noted below), are eligible for reimbursement for ambulatory surgery services provided in ASCs. We propose to accept Medicare's determination of a facility as an ASC. If the facility meets the definition of an ASC at 42 CFR 416.2 and has an agreement with Medicare as an ASC, we propose that they will be considered an authorized ASC under TRICARE and subject to all requirements for authorized institutional provider status under 32 CFR 199.6. ASCs must also enter into a participation agreement with TRICARE, to ensure that the ASC accepts the TRICARE reimbursement rate, and meets all other conditions of coverage. Additionally, due to the differences between the TRICARE and Medicare populations, there may be ASCs that specifically serve pediatric populations. These ASCs may not routinely enter into agreements with Medicare. We propose that these facilities may also be reimbursed under this proposed system, but they must be accredited by the Joint Commission, the Accreditation Association for Ambulatory Health Care, Inc. (AAAHC), or have other accreditation as authorized by the Director, DHA and published in the implementing instructions. Additionally, these facilities must also enter into participation agreements with TRICARE in order to receive reimbursement under the program. Facilities that do not participate under Medicare, or are otherwise accredited, and do not have participation agreements with TRICARE as noted above, shall not be TRICARE authorized providers and will not receive reimbursement for ambulatory surgery services. We do not believe that this requirement will have any impact on access to care, as ambulatory surgery services are also available in hospital outpatient departments. We believe that the flexibility offered to pediatric specialty ASCs is sufficient to serve the unique needs of our patient population, while still ensuring the program complies with the requirements of 10 U.S.C. 1079 (i). These TRICARE-certified pediatric ASCs will be subject to the same reimbursement system as proposed in this regulatory action.
What is the Medicare reimbursement system for ambulatory surgery centers?
1. Adopting Medicare's Ambulatory Surgical Center Reimbursement System for TRICARE Authorized Ambulatory Surgery Centers. Per Title 10 United States Code (U.S.C.), 1079 (i) (2), TRICARE's payment methods for institutional care shall be determined, to the extent practicable, in accordance with the same reimbursement rules used by Medicare. Under this proposed rule, TRICARE will reimburse ASCs for ambulatory surgical services using a method similar to Medicare's ASC reimbursement methodology. Under the proposed TRICARE ASC reimbursement method, payment for a TRICARE patient will be made at the lower of the billed charge or the Medicare-determined ASC payment rate with applicable TRICARE Start Printed Page 65719 cost-sharing provisions. The TRICARE ASC reimbursement method would include payment for all facility services associated with the surgical procedure that are included in the payment methodology by Medicare, but would exclude certain services also excluded by Medicare under the ASC reimbursement methodology ( e.g., certain ancillary services and implantable devices with pass-through status).
When did Medicare replace ASC?
Medicare replaced their previous ASC system on January 1, 2008. Medicare's reimbursement system for ASCs uses OPPS relative payment rates as a guide. OPPS rates are reduced by a factor to account for the fact that ASCs have lower overhead costs than hospitals. In 2012, Medicare's ASC rates averaged 61 percent of the OPPS rates paid to acute care hospitals for surgical procedures. Under Medicare, ASCs are paid the lesser of the billed charge or the standard ASC reimbursement rate, a method which TRICARE proposes to adopt.
What is reduced payment tricare?
Reduced payments are made for certain procedures when a specified device is furnished without cost or for which either a partial or full credit is received ( e.g., device recall). TRICARE proposes to adopt this methodology as well as any other future refinements or adjustments to this methodology.
Does Tricare pay for multiple procedures?
TRICARE proposes adopting the same methodology for payment of multiple procedures as Medicare, as well as adopting all future refinements and adjustments. When multiple procedures are performed in the same operative session that are subject to the multiple procedure discount, 100% of the highest paying surgical procedure on the claim is paid, plus 50% of the applicable payment rates for the other ASC covered surgical services. The CMS OPPS/ASC annual final rules specify the surgical procedures subject to multiple discounting, which TRICARE proposes to adopt. In determining the ranking of the procedures for the discounting, the lower of the billed charge or the ASC payment amount will be used.
Step 1 - Identify the Locality
Procedure pricing is calculated based on locality. Enter a ZIP Code, select a State, or specify a Foreign Country.
Step 2 - Keyword or Provider Search
If you'd like you can limit the provided data using the filter options below.
How much of a TRICARE payment can a non-participating provider bill?
Nonparticipating providers may only bill the beneficiary up to 115 percent of the TRICARE allowed amount. If the OHI paid more than 115 percent of the allowed amount, no TRICARE payment is authorized, as the charge is considered paid in full and the provider may not bill the beneficiary. Otherwise, TRICARE pays the lower of:
What is the billed amount minus the OHI payment?
the billed amount minus the OHI payment. the amount TRICARE would have paid without OHI. the amount the beneficiar y owes after the OHI paid (usually the OHI copayment or cost-share) Non-network providers who do not accept TRICARE assignment (nonparticipating)
Does tricare pay OHI?
TRICARE requires coordination of benefits with other health insurance (OHI) coverage. TRICARE does not always pay the beneficiary’s OHI copayment or the balance left over after the OHI payment. However, the beneficiary usually owes very little to nothing.
