Benefits With Medicare Coverage Limits
- Medicare Part A Lifetime Limits. Medicare Part A covers hospital stays for any single illness or injury up to a benefit period of 90 days.
- Mental Health Benefits and Psychiatric Hospital Stays. Medicare only covers 190 days of inpatient care in a psychiatric hospital throughout your lifetime. ...
- Skilled Nursing Facilities. ...
- Therapy Services. ...
What are the limitations of Medicare?
- death of a spouse
- divorce
- marriage
- working fewer hours
- retiring or losing your job
- loss of income from another source
- loss or reduction of pension
Does Medicare have lifetime limits?
Medicare Part A covers hospital stays for any single illness or injury up to a benefit period of 90 days. If you need to stay in the hospital more than 90 days, you have the option of using your lifetime reserve days, of which the Medicare lifetime limit is 60 days.
What is the lifetime cap on Medicare?
Skilled Nursing Facilities
- Up to 20 days: Medicare pays the full cost
- From day 21-100: you pay a share of the cost ($185.50 coinsurance per day of each benefit period in 2021)
- Beyond 100 days: you pay all costs.
What are the income limits for Medicare?
- When it comes to receiving Medicare benefits, there are no income restrictions.
- You may be asked to pay more money for a premium depending on your income.
- If you have a minimal income, you may be eligible for Medicare premium assistance.

What is the Medicare threshold for 2021?
Here's how much higher-income Medicare beneficiaries will pay for coverage in 2021. Next year, the income-related monthly adjustments will kick in for individuals with modified adjusted gross income above $88,000. For married couples who file a joint tax return, that threshold is $176,000.
How much money can you make before it affects Medicare?
To qualify, your monthly income cannot be higher than $1,010 for an individual or $1,355 for a married couple. Your resource limits are $7,280 for one person and $10,930 for a married couple. A Qualifying Individual (QI) policy helps pay your Medicare Part B premium.
Does Social Security count as income for Medicare?
All types of Social Security income, whether taxable or not, received by a tax filer counts toward household income for eligibility purposes for both Medicaid and Marketplace financial assistance.
Can you be denied Medicare?
In all but four states, insurance companies can deny private Medigap insurance policies to seniors after their initial enrollment in Medicare because of a pre-existing medical condition, such as diabetes or heart disease, except under limited, qualifying circumstances, a Kaiser Family Foundation analysis finds.
What are Medicare income limits?
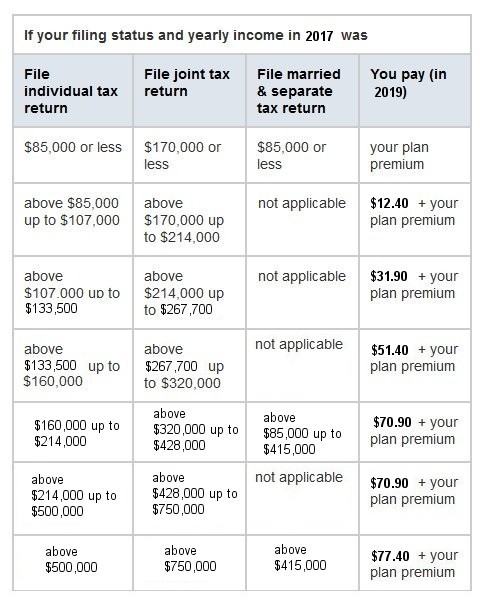
Medicare beneficiaries with incomes above a certain threshold are charged higher premiums for Medicare Part B and Part D. The premium surcharge is...
Why does Medicare impose income limits?
The higher premiums for Part B took effect in 2007, under the Medicare Modernization Act. And for Part D, they took effect in 2011, under the Affor...
Who is affected by the IRMAA surcharges and how does this change over time?
There have been a few recent changes that affect high-income Medicare beneficiaries: In 2019, a new income bracket was added at the high end of the...
Will there be a rate increase in 2022?
We don’t yet have concrete details from CMS. But the Medicare Trustees Report, which was published in late August, projects that the standard Part...
How much does Medicare pay for therapy?
Starting in 2019, Medicare no longer limits how much it will pay for medically necessary therapy services. You will typically pay 20% of the Medicare-approved amount for your therapy services, once you have met your Part B deductible for the year.
How long does Medicare cover psychiatric care?
Medicare only covers 190 days of inpatient care in a psychiatric hospital throughout your lifetime. If you require more than the Medicare-approved stay length at a psychiatric hospital, there’s no lifetime limit for mental health treatment you receive as an inpatient at a general hospital.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) cover inpatient hospital and outpatient health care services that are deemed medically necessary. " Medically necessary " can be defined as “services and supplies that are needed to prevent, diagnose, or treat illness, injury, disease, health conditions, ...
What is a Medigap policy?
Medicare Supplement Insurance (Medigap) policies are private health care plans designed to supplement your Original Medicare benefits and help pay for some of the out-of-pocket costs that Original Medicare doesn’t cover.
How long can you stay in a hospital with Medicare?
Medicare Part A covers hospital stays for any single illness or injury up to a benefit period of 90 days. If you need to stay in the hospital more than 90 days, you have the option of using your lifetime reserve days, of which the Medicare lifetime limit is 60 days.
What are the services that are beyond the annual limit?
Extended hospitalization. Psychiatric hospital stays. Skilled nursing facility care. Therapy services. If you require any of these services beyond the annual limits, and don't qualify for an exception, you may be responsible for the full cost of those services for the rest of the year.
Does Medicare cover skilled nursing facilities?
Skilled Nursing Facilities. For Medicare to cover skilled nursing facility care, you must be formally admitted to the hospital with a doctor's order. Even so, there are limits to the coverage your Medicare benefits provide.
What is the Medicare donut hole?
Medicare Part D prescription drug plans feature a temporary coverage gap, or “ donut hole .”. During the Part D donut hole, your drug plan limits how much it will pay for your prescription drug costs. Once you and your plan combine to spend $4,130 on covered drugs in 2021, you will enter the donut hole. Once you enter the donut hole in 2021, you ...
How much is Medicare Part A deductible in 2021?
You are responsible for paying your Part A deductible, however. In 2021, the Medicare Part A deductible is $1,484 per benefit period. During days 61-90, you must pay a $371 per day coinsurance cost (in 2021) after you meet your Part A deductible.
What happens if you spend $6,550 out of pocket in 2021?
After you spend $6,550 out-of-pocket on covered drugs in 2021, you leave the donut hole coverage gap and enter the catastrophic coverage stage. Once you reach this stage, you only pay a small coinsurance or copayment for your covered drugs for the rest of the year.
What is Medicare Part B and Part D?
Medicare Part B (medical insurance) and Part D have income limits that can affect how much you pay for your monthly Part B and/or Part D premium. Higher income earners pay an additional amount, called an IRMAA, or the Income-Related Monthly Adjusted Amount.
What is Medicare Advantage Plan?
When you enroll in a Medicare Advantage plan, it replaces your Original Medicare coverage and offers the same benefits that you get from Medicare Part A and Part B.
How long does Medicare cover hospital care?
Depending on how long your inpatient stay lasts, there is a limit to how long Medicare Part A will cover your hospital costs. For the first 60 days of ...
How many reserve days do you get with Medicare?
Medicare limits you to only 60 of these days to use over the course of your lifetime, and they require a coinsurance payment of $742 per day in 2021. You only get 60 lifetime reserve days, and they do not reset after a benefit period or a calendar year.
How does Medicare determine premiums?
To determine the premiums it assigns, Medicare uses someone’s federal tax return from the Internal Revenue Service (IRS). In figuring the premiums of beneficiaries for 2021, Medicare uses tax returns from 2019, which is the most recent year the IRS provides to Social Security. Most of the income thresholds for premium adjustments are subject ...
What are the two Medicare programs that require higher monthly premiums?
Those with higher incomes must pay higher monthly premiums for two Medicare programs. These include Part B , which is the outpatient medical coverage of original Medicare, and Part D , the program that provides prescription drug coverage. This article discusses the parts of Medicare that higher premiums may, or may not, affect.
What is Medicare supplement insurance?
This plan combines the benefits of original Medicare parts A and B into one policy. Medigap, which is Medicare supplement insurance. This plan is available for purchase to a person with original Medicare. Private insurance companies administer both Medicare Advantage and Medigap plans.
How to appeal Medicare premium adjustment?
If an individual does not agree with Medicare’s decision about their income-related premium adjustment, they can file an appeal. To do this, a person may call Social Security at 800-772-1213. A deaf or partially deaf person may call 877-486-2048.
What is the standard rate for Medicare 2021?
The majority of people fall into the income range associated with the standard rate, which in 2021 is $148.50. This amount can change each year.
When will premium adjustments be changed?
Most of the income thresholds for premium adjustments are subject to change. Starting in 2020 , the government will change all the thresholds every year to reflect general price inflation. The only exception to these changes is the threshold for the top income level.
Can income be high for Medicare?
A person’s income cannot be so high that it disqualifies them for Medicare. Even those who receive very high incomes may enroll. However, individuals with higher incomes pay higher premiums for parts B and D, but Medicare income limits that affect premium rates only affect a small percentage of people.
All U.S. citizens aged 65 and older qualify for Medicare, regardless of income
We want to start by saying that Medicare eligibility is not based on income. If you are an American citizen age 65 or older, you qualify for Medicare. How much money you do or do not make plays no part. Some people confuse Medicare with Medicaid, which does have an income requirement.
How Do You Qualify for Medicare?
The majority of beneficiaries – around 85 percent – qualify for Medicare based on their age. All American citizens aged 65 or older can sign up for Medicare.
Does Income Affect Medicare Part A Premiums?
Medicare Part A, also known as hospital insurance, covers inpatient care. The vast majority of Medicare beneficiaries paid payroll taxes for the required 40 quarters (10 years) to qualify for premium-free Part A. Even if you do have a Medicare Part A premium, though, you won't pay more based on your income.
How Income Affects Medicare Part B Premiums
Medicare Part B is also known as medical insurance. It covers services like doctor visits and lab work. The standard Medicare Part B premium is $170.10 per month in 2022.
How Income Affects Medicare Part D Premiums
Original Medicare does not include prescription drug coverage. These benefits are available through a Medicare Part D prescription drug plan (PDP). You may join either a standalone Part D plan or a Medicare Advantage Prescription Drug plan (MA-PD).
How Medicare Determines IRMAA
Medicare premiums are based on the adjusted gross income you reported to the IRS two years ago. You will receive the IRMAA notification from Social Security if your MAGI exceeds the amounts listed above.
How to Qualify for Help Paying Your Medicare Parts A and B Costs
There are four Medicare Savings Programs designed to help beneficiaries pay their Medicare costs. This may include deductibles, coinsurance, and copayments. Guidelines for each program vary.
What is the tax rate for Social Security?
The current tax rate for social security is 6.2% for the employer and 6.2% for the employee, or 12.4% total. The current rate for Medicare is 1.45% for the employer and 1.45% for the employee, or 2.9% total. Refer to Publication 15, (Circular E), Employer's Tax Guide for more information; or Publication 51, (Circular A), Agricultural Employer’s Tax Guide for agricultural employers. Refer to Notice 2020-65 PDF and Notice 2021-11 PDF for information allowing employers to defer withholding and payment of the employee's share of Social Security taxes of certain employees.
What is the FICA 751?
Topic No. 751 Social Security and Medicare Withholding Rates. Taxes under the Federal Insurance Contributions Act (FICA) are composed of the old-age, survivors, and disability insurance taxes, also known as social security taxes, and the hospital insurance tax, also known as Medicare taxes. Different rates apply for these taxes.
What is the wage base limit for 2021?
The wage base limit is the maximum wage that's subject to the tax for that year. For earnings in 2021, this base is $142,800. Refer to "What's New" in Publication 15 for the current wage limit for social security wages; or Publication 51 for agricultural employers. There's no wage base limit for Medicare tax.
How long does it take to pay Medicare premiums if income is higher than 2 years ago?
If your income two years ago was higher and you don’t have a life-changing event that makes you qualify for an appeal, you will pay the higher Medicare premiums for one year. IRMAA is re-evaluated every year as your income changes.
What percentage of Medicare premiums do Medicare beneficiaries pay?
The premiums paid by Medicare beneficiaries cover about 25% of the program costs for Part B and Part D. The government pays the other 75%.
How many income brackets are there for IRMAA?
As if it’s not complicated enough for not moving the needle much, IRMAA is divided into five income brackets. Depending on the income, higher-income beneficiaries pay 35%, 50%, 65%, 80%, or 85% of the program costs instead of 25%. The lines drawn for each bracket can cause a sudden jump in the premiums you pay.
What is the income used to determine IRMAA?
The income used to determine IRMAA is your AGI plus muni bond interest from two years ago. Your 2020 income determines your IRMAA in 2022. Your 2021 income determines your IRMAA in 2023. The untaxed Social Security benefits aren’t included in the income for determining IRMAA. As if it’s not complicated enough for not moving the needle much, ...
How much does Medicare cover?
The premiums paid by Medicare beneficiaries cover about 25% of the program costs for Part B and Part D. The government pays the other 75%. Medicare imposes surcharges on higher-income beneficiaries. The theory is that higher-income beneficiaries can afford to pay more for their healthcare. Instead of doing a 25:75 split with ...
How much does Medicare premium jump?
If your income crosses over to the next bracket by $1, all of a sudden your Medicare premiums can jump by over $1,000/year. If you are married and both of you are on Medicare, $1 more in income can make the Medicare premiums jump by over $1,000/year for each of you.
When will IRMAA income brackets be adjusted for inflation?
The IRMAA income brackets (except the very last one) started adjusting for inflation in 2020. Here are the IRMAA income brackets for 2021 coverage and the projected brackets for 2022 coverage. Before the government publishes the official numbers, I’m able to make projections based on the inflation numbers to date.
