Non-medical care is best defined as care or assistance provided by individuals without formal medical training. It Is Important to grasp the distinction between non-medical and medical care, as doing so helps families to better understand and utilize their health insurance benefits and find financial assistance to care for a loved one.
Full Answer
Can I use private insurance instead of Medicare?
You can also have both Medicare and private insurance to help cover your health care expenses. In situations where there are two insurances, one is deemed the “primary payer” and pays the claims first. The other becomes known as the “secondary payer” and only applies if there are expenses not covered by the primary policy.
What are the top 5 Medicare supplement plans?
- Plan G
- Plan N
- Plan A
- Plan F
- High Deductible Plan F
How is Medicare different from private insurance?
- Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments.
- Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. ...
- Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. ...
Why are Medicare Advantage plans bad?
What is a non-participating provider Medicare?
Non-participating providers haven't signed an agreement to accept assignment for all Medicare-covered services, but they can still choose to accept assignment for individual services. These providers are called "non-participating."
What is non Medicare plan?
Primary Plan: ECP The Enhanced Care PPO (ECP) plan is the primary plan for non-Medicare Trust members. This nationwide health plan provides unlimited primary care physician (PCP) and specialist physician office visits at a flat dollar copay, as well as other helpful programs.
What types of healthcare are not covered by Medicare?
In general, Original Medicare does not cover:Prescription drugs.Long-term care (such as extended nursing home stays or custodial care)Hearing aids.Most vision care, notably eyeglasses and contacts.Most dental care, notably dentures.Most cosmetic surgery.Massage therapy.More items...•
How does Medicare differ from non Medicare?
Medicare is a federal program that provides health coverage if you are 65+ or under 65 and have a disability, no matter your income. Medicaid is a state and federal program that provides health coverage if you have a very low income.
What is meant by Medicare?
/ˈmedɪkeər/ us. in the US, a government program that pays for medical treatment for people aged 65 or over: Medicare programs/reforms/benefits. Medicare patients/recipients/beneficiaries. in Australia, the national system that provides medical treatment, which is paid for by taxes.
Is Cigna Medicare or non Medicare?
Cigna offers Medicare Advantage plans in 16 states and Washington, D.C, and Medicare Prescription Drug Plans in all 50 states. Cigna's Medicare Supplement Insurance (Medigap) plans are available in every state but Massachusetts and New York.
Can we bill Medicare patients for non covered services?
Under Medicare rules, it may be possible for a physician to bill the patient for services that Medicare does not cover. If a patient requests a service that Medicare does not consider medically reasonable and necessary, the payer's website should be checked for coverage information on the service.
What is the difference between Medicare and Medicaid?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
Does Medicare pay for everything?
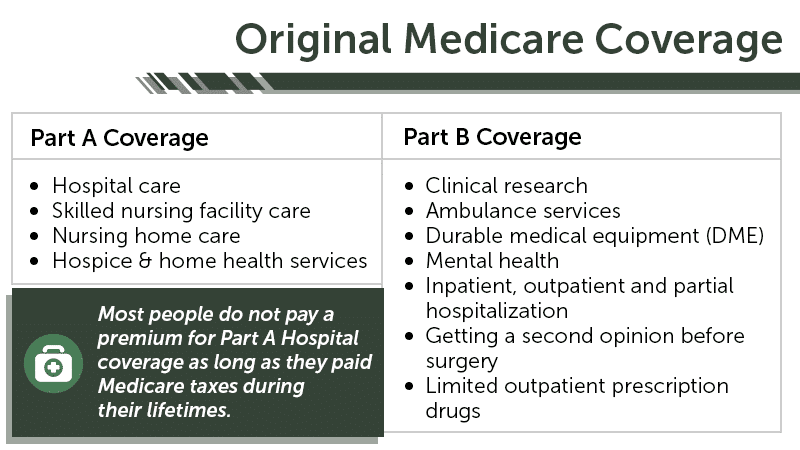
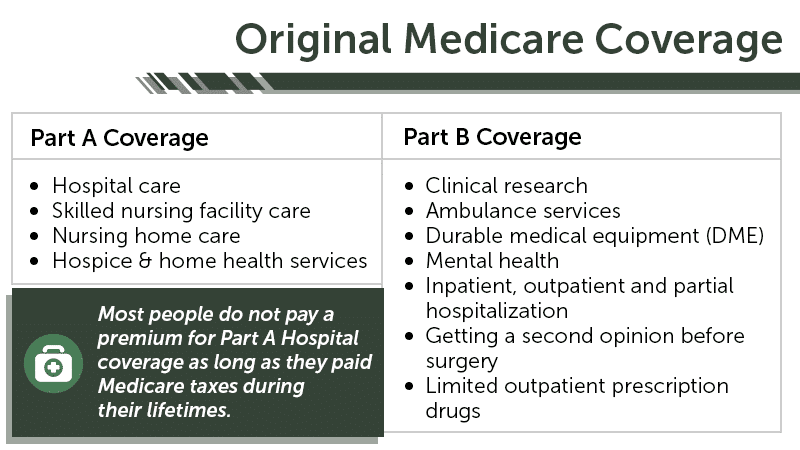
Basic, or original, Medicare consists of two parts: Part A and Part B. Part A provides coverage for hospital stays, skilled nursing, hospice and some home health services. As long as you have at least a 10-year work history, you pay nothing for Part A.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Who pays for Medicaid?
The Medicaid program is jointly funded by the federal government and states. The federal government pays states for a specified percentage of program expenditures, called the Federal Medical Assistance Percentage (FMAP).
Does everyone get Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
How much can non-participating providers charge for Medicare?
Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
What does it mean to take assignment with Medicare?
Taking assignment means that the provider accepts Medicare’s approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive.
What happens if you pay Medicare up front?
If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount.
How long does it take for a provider to bill Medicare?
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you.
Does Medicare charge 20% coinsurance?
However, they can still charge you a 20% coinsurance and any applicable deductible amount. Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Do opt out providers accept Medicare?
Opt-out providers do not accept Medicare at all and have signed an agreement to be excluded from the Medicare program. This means they can charge whatever they want for services but must follow certain rules to do so. Medicare will not pay for care you receive from an opt-out provider (except in emergencies).
Can you have Part B if you have original Medicare?
Register. If you have Original Medicare, your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare.
How much can a non-participating provider bill Medicare?
Medicare will then send any reimbursement directly to the patient. As a Non-Participating Medicare Provider, you can bill the patient up to 115% of the Medicare Fee Schedule.
What is the most common Medicare Advantage plan?
There are coordinated care options such as HMOs or PPOs, private fee-for-service (PFFS) plans, and medical savings account (MSA) plans. The most common form of Medicare Advantage plan is the HMO. Apparently, there are a number of Medicare Advantage plans in which coverage is limited to only in-network providers.
What is the maximum amount of Medicare Physician Fee Schedule?
If you are a Non-Participating provider, providing covered services and collecting payment from beneficiaries at the time of service, the maximum amount you may charge is 115% of the approved fee schedule amount for Non-Participating providers; which is 95% of the normal Medicare Physician Fee Schedule (MPFS).
What is the relationship status of a physical therapist with Medicare?
There are three possibilities for a Physical Therapist’s relationship-status with Medicare: 1) No relationship at all (notthe same as a “Non-Participating Provider” and also notthe same as “opting out”) 2) Participating Provider. 3) Non-Participating Provider.
Can a Medicare beneficiary see you out of network?
If a beneficiary with a Medicare Advantage plan wants to see you on a cash-pay basis, and you are out-of-network with that plan , you need to call the plan and ask them if it is okay for you to provide them with covered services and that the beneficiary pay you directly out-of-pocket.
Can you bill Medicare if you are not a par?
A little more detail on the Non-Par Status: You can accept self-payment from the beneficiary at the time of service, but you still must send in the claim to Medicare. Medicare will then send any reimbursement directly to the patient. As a Non-Participating Medicare Provider, you can bill the patient up to 115% of the Medicare Fee Schedule.
Can non-par providers take payment in full?
This is hugely important for some practices in certain areas with certain demographics. Non-Par Providers can also take payment in full at the time of service directly from the beneficiary, so they are not waiting for a 3rd Party Payor to reimburse them.
What does it mean when a doctor is a non-participating provider?
If your doctor is what’s called a non-participating provider, it means they haven’t signed an agreement to accept assignment for all Medicare-covered services but can still choose to accept assignment for individual patients . In other words, your doctor may take Medicare patients but doesn’t agree to ...
What does Medicare status mean?
Your doctor's Medicare status determines how much Medicare covers and your options for finding lower costs.
Why are doctors dropping Medicare?
Thanks to plummeting reimbursement rates, ever-tightening rules, and cumbersome paperwork, many doctors are dropping Medicare. If you recently enrolled in Medicare only to find that your long-standing doctor doesn’t accept it, you have a number of options.
How much is Medicare Part B 2021?
All you’ll likely have to pay is the monthly Medicare Part B premium ($148.50 base cost in 2021) and the annual Part B deductible: $203 for 2021. 6 As a Medicare patient, this is the ideal and most affordable scenario.
How many people were in Medicare in 1965?
President Lyndon B. Johnson signed Medicare into law on July 30, 1965. 1 By 1966, 19 million Americans were enrolled in the program. 2 . Now, more than 50 years later, that number has mushroomed to over 60 million; more than 18% of the U.S. population.
Will all doctors accept Medicare in 2021?
Updated Jan 26, 2021. Not all doctors accept Medicare for the patients they see, an increasingly common occurrence. This can leave you with higher out-of-pocket costs than you anticipated and a tough decision if you really like that doctor.
Do doctors take Medicare?
There are still plenty of doctors who take Medicare. You can find them in Medicare’s Physician Compare directory, a comprehensive list of physicians and healthcare providers across the nation. Once you pinpoint a provider, call to make sure they’re still taking on new Medicare patients. After all, this can change on a dime.
What services does Medicare cover?
Dentures. Cosmetic surgery. Acupuncture. Hearing aids and exams for fitting them. Routine foot care. Find out if Medicare covers a test, item, or service you need. If you need services Medicare doesn't cover, you'll have to pay for them yourself unless you have other insurance or a Medicare health plan that covers them.
Does Medicare cover everything?
Medicare doesn't cover everything. Some of the items and services Medicare doesn't cover include: Long-Term Care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Does Medicare pay for long term care?
Medicare and most health insurance plans don’t pay for long-term care. (also called. custodial care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom.
What does "non-par" mean in Medicare?
Non-PAR stands for non-participating. You are enrolled in Medicare but are not under contract with the Agency, so you must agree to receive payment for the services you provide to Medicare patients differently than a Medicare participating provider. Not being constrained by a Medicare contract allows you to choose whether to accept assignment.
How much less is a non-PAR provider than a Medicare provider?
However, there are some differences. As a non-PAR provider accepting assignment, you are paid 5% less than a Medicare participating provider. Also, to collect the 20% that Medicare doesn’t cover, you must go directly to the patient versus being able to bill their secondary insurance.
What is PAR provider contract?
As part of your PAR provider contract, your practice agrees to take assignment on all Medicare claims. This means you must accept the amount that Medicare assigns for payment for the services you provide.
What happens if you choose the wrong Medicare provider?
Choosing the wrong Medicare participation status for your provider can have significant financial consequences for your practice. Your choices are a Medicare Participating Provider (PAR) or a Medicare Non-Participating Provider (non-PAR). If you make the wrong choice, your allowable reimbursement can be limited, ...
How often does Medicare revalidate?
In addition to enrollment, the revalidation process – which occurs every five years in Medicare’s Provider Enrollment, Chain and Ownership System (PECOS) – also requires you to choose your participation status. Failure to revalidate can lead to deactivation from Medicare and the loss of reimbursement funds.
What is Medicare Participating Provider?
What is a Medicare Participating Provider? Enrolling as a Medicare participating provider means that you are in-network with the plan. You may also see this listed as a PAR provider. PAR stands for participating, and as such, your practice has a contract with Medicare.
What does it mean to not be constrained by Medicare?
Not being constrained by a Medicare contract allows you to choose whether to accept assignment. This means choosing whether you’ll be paid by Medicare or the patient. You can choose your assignment designation on a claim-by-claim basis or for each of the Medicare claims you submit. Only non-PAR providers have this option.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.