What is the Amt field on the GRP/RC?
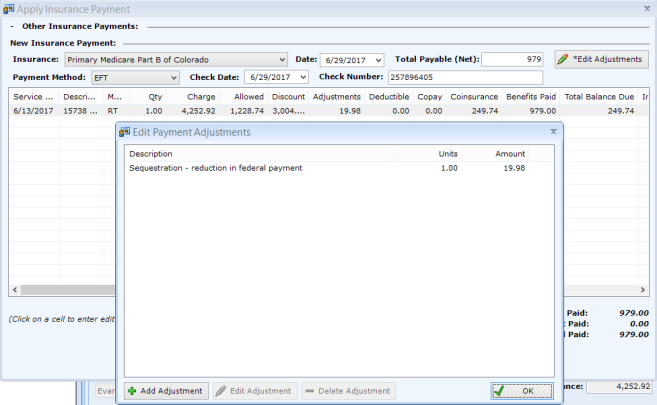
Group/Reason Code Amount (GRP/RC - AMT): The AMT field contains the amount of any adjustment that was made based on the preceding Group Code and CARC.
What does GRP/RC-Amt stand for?
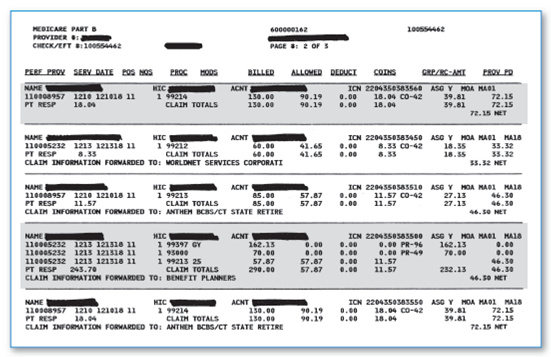
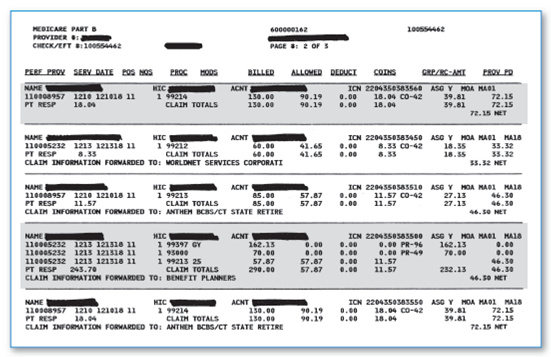
Reason codes (RC) and amount of adjustments are printed under the "GRP/RC-AMT" column. Under the standard format, only the claim adjustment reason codes approved by the American National Standards Institute (ANSI) X12 835 Insurance Subcommittee are printed under the "GRP/RC-AMT" column.
What does GRP stand for in billing?
Group (GRP) Values: (1) PR – Patient Responsibility: This signifies the amount that may be billed to the beneficiary or to another payer on the beneficiary's behalf. Providers may be subject to penalties if they bill a patient for charges not identified with the PR group code.
What is the difference between GRP/RC-Amt and claim adjustment reason codes?
Reason codes (RC) and amounts of adjustments are printed under the "GRP/RC-AMT" column. Under the standard format, only the claim adjustment reason codes approved by the American National Standards Institute (ANSI) X12 835 Insurance Subcommittee are printed under the "GRP/RC-AMT" column.
What is total RC AMT on Medicare EOB?
Total RC-Amt: Total amount of non-covered services. This is the difference between the total billed amount and the total allowed amount.
What is RC AMT?
TOTAL RC -AMT. This field indicates the total amount of adjustments made to assigned claims due to Claim Adjustment Reason Codes (CARCs) listed on each service line. This excludes interest, late filing charges, deductibles, and amounts previously paid for rendered services.
What is GRP in medical billing?
Group Reason Code (GRP/RC): Group codes represent the financially responsible party. Reason codes explain denials and payments. These combination of codes are defined in the glossary at the bottom of the Standard Provider Remittance.
What does Medicare RTP mean?
Return to ProviderWhen a claim is submitted, it processes through a series of edits in the Fiscal Intermediary Standard System (FISS), to ensure the information submitted is complete and correct. If the claim has incomplete, incorrect or missing information, it will be sent to your return to provider (RTP) file.
What is the difference between an EOB and an RA?
Difference of Recipient Both types of statements provide an explanation of benefits, but the remittance advice is provided directly to the health-care provider, whereas the explanation of benefits statement is sent to insured patient, according to Louisiana Department of Health.
What is a claim payment remittance advice and check?
An electronic remittance advice, or ERA, is an explanation from a health plan to a provider about a claim payment. An ERA explains how a health plan has adjusted claim charges based on factors like: Contract agreements. Secondary payers. Benefit coverage.
What are Medicare CARC codes?
Claim Adjustment Reason CodesClaim Adjustment Reason Codes (CARCs) are used on the Medicare electronic and paper remittance advice, and Coordination of Benefit (COB) claim transaction. The Claim Adjustment Status and Reason Code Maintenance Committee maintains this code set.
What does CARC mean on Medicare EOB?
Claim Adjustment Reason CodeClaim Adjustment Reason Code (CARC)
What is the difference between claim level and line level?
Data should be reported at the higher level with the Claim Level being the higher level and the Line Level being the lower level. Claim Level data reported is accepted for all lines of service in the claim and any information reported at the Line Level supersedes the data reported at the Claim Level.
What are the denial codes?
1 – Denial Code CO 11 – Diagnosis Inconsistent with Procedure. ... 2 – Denial Code CO 27 – Expenses Incurred After the Patient's Coverage was Terminated. ... 3 – Denial Code CO 22 – Coordination of Benefits. ... 4 – Denial Code CO 29 – The Time Limit for Filing Already Expired. ... 5 – Denial Code CO 167 – Diagnosis is Not Covered.
What are return to provider codes?
The “return to provider” codes include symptom codes that may be used by physical, occupational, and speech therapists as treatment diagnoses on their plans of care.
What does reason code mean?
Reason codes, also called score factors or adverse action codes, are numerical or word-based codes that describe the reasons why a particular credit score is not higher. For example, a code might cite a high utilization rate of available credit as the main negative influence on a particular credit score.
What is the HIC number on an EOB?
The “HIC” number is the member’s personal identification number that the insurance company uses to identify them.
What is an ACCT number?
The “ACCT” number is a blend of the patient’s account number from the physician’s records and an assigned number from the insurance company. The internal control number or “ICN” is the number assigned by the insurance company that identifies the claim. The ICN will be asked for anytime you communicate with your insurance company about ...
How much is deductible for insurance?
Many insurance plans have a “deductible,” or a set amount that the patient is responsible for each year. If your plan has a $200 deductible, then starting January 1 st each year, your responsibility of $200 begins again and the insurance company will not pay anything to your physician until you have paid the $200.
Where is the glossary reference on EOB?
The “GLOSSARY” reference at the bottom of the EOB will give a short explanation of each code referenced in the EOB. After the primary insurance and secondary insurance have processed the claims, finally, the physician will send a bill for any leftover patient responsibility to the patient.
What is the most common EOB format?
The most common format style used is the Standard Paper Remittance format. This format is most commonly used by Medicare.
What is an EOB?
Understanding an EOB and Your Bill. An Explanation of Benefits (EOB) is the document that health insurance companies send to communicate their decisions to members regarding payment for services. Every insurance company EOB is different, and many of them are difficult to understand. An EOB is not a bill, but it usually will have enough information ...
What does it mean when a doctor accepts an insurance payment?
If you have received services from a ‘preferred’ or ‘in-network’ provider, that means the doctor has a contract with your insurance company to accept the amount the insurance company is willing to pay for services. The amount the company is willing to pay is known as the “allowed amount”.
What is ASC X12 835?
A particular ASC X12 835 reason or remark code might be mapped to one or more shared system codes, or vice versa, making it difficult for a MAC to determine each of the internal codes that may be impacted by remark or reason code modification, retirement, or addition.
What is reason and remark code?
In most cases, reason and remark codes reported in remittance advice transactions are mapped to alternate codes used by a shared system. These shared system codes may exceed the number of the reason and remark codes approved for reporting in a remittance advice transaction.
What is Medicare group code?
Medicare Group Codes. A group code is a code identifying the general category of payment adjustment. A group code must always be used in conjunction with a claim adjustment reason code to show liability for amounts not covered by Medicare for a claim or service. MACs do not have discretion to omit appropriate codes and messages.
What is a group code in CARC?
Group codes are codes that will always be shown with a reason code to indicate when a provider may or may not bill a beneficiary for the non-paid balance of the services furnished. Payment Adjustment Category Description. • PR (Patient Responsibility).
Can deactivated code be used in derivative business messages?
The Shared System Maintainers shall make sure that a deactivated code (either reason or remark) is not allowed to be used in any original business message, but is allowed and processed when reported in derivative business messages.
Do you need separate reason codes in the NSF?
Separate reason code entries must be used in the NSF for the CR group entry and any other groups that apply to the readjudicated claim. At least one reason code is always used with a group code in the NSF .