The Medicare case-mix index (CMI) reflects the costliness of a hospital's Medicare patient mix. The costs are based on the diagnosis-related group (DRG) in which each patient is classified and the weight that Medicare has applied to each DRG to reflect patients' relative costs.
What is the Medicare case mix index (CMI)?
The Medicare case-mix index (CMI) reflects the costliness of a hospital's Medicare patient mix. The costs are based on the diagnosis-related group (DRG) in which each patient is classified and the weight that Medicare has applied to each DRG to reflect patients' relative costs.
What is case mix in home health?
National Association of Home Care and Hospice (NAHC) has a small explainer of key terms in home health. NAHC defines it as “Case Mix—term used to identify resource use for Medicare providers.
What is the relationship between case mix index and reimbursement?
Higher case mix index values indicate that a hospital has treated a greater number of complex, resource-intensive patients, and the hospital will be reimbursed at a higher rate.
What does a lower case mix index indicate?
Though the patients that they care for and the services that they provide are largely the same, a lower case mix index could indicate that one hospital is documenting its cases less effectively. It’s important to remember, however, that this metric can be impacted by many different factors, including:
What is a case mix in healthcare?
The Case Mix Index (CMI) is the average relative DRG weight of a hospital's inpatient discharges, calculated by summing the Medicare Severity-Diagnosis Related Group (MS-DRG) weight for each discharge and dividing the total by the number of discharges.
What is the meaning of case mix?
The term case-mix refers to the type or mix of patients treated by a hospital or unit. The term is often used to describe the billing system of the hospital or unit, since the "cost per item" of health care is based on the case-mix.
What is a good case mix index?
CMI for the top 25 hospitals range from 3.23 to 5.69 with an average CMI of 3.78. There was a slight increase from the average CMI of 3.48 for the top hospitals in 2018. With patients delaying care during the COVID-19 pandemic, hospitals were seeing the most severe patients, potentially increasing CMIs.
What is case mix classification?
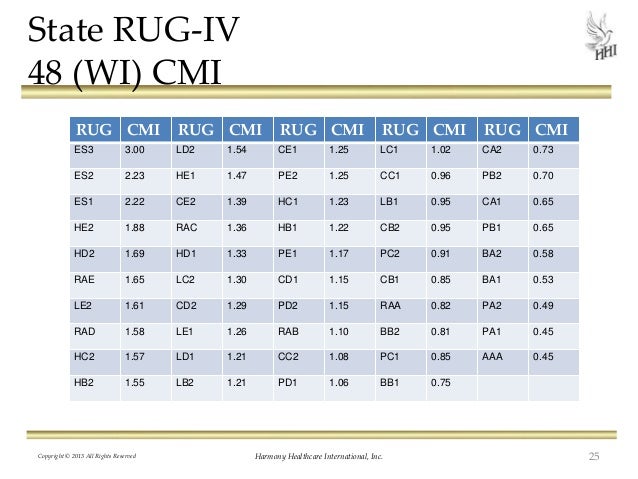
What is Case Mix? Minnesota Case Mix is a system that classifies residents into distinct groups called Resource Utilization Groups (RUGs) based on the resident's condition and the care the resident was receiving at the time of the assessment.
What is case-mix payment?
Case Mix Adjustment: Payments under the SNF PPS are case-mix adjusted in order to reflect the relative resource intensity that would typically be associated with a given patient's clinical condition, as identified through the resident assessment process.
Why is CMI important?
CMI is an important performance indicator for your hospital not because it tells a big story in and of itself, but because of how it impacts your hospital's finances. CMI is a measure of the average severity level of a hospital's procedures.
What determines CMI?
A hospital's CMI represents the average diagnosis-related group (DRG) relative weight for that hospital. It is calculated by summing the DRG weights for all Medicare discharges and dividing by the number of discharges. CMIs are calculated using both transfer-adjusted cases and unadjusted cases.
How do I increase my CMI?
Five Ways to Improve Case-Mix Index For Your CommunityHold CMI Review Meetings. ... Communicate with Therapy. ... Capture the Complete Clinical Picture. ... Accurately Code Activities of Daily Living. ... Complete Interviews Timely and Accurately.
What affects CMI?
What many organizations are failing to acknowledge is changing admission patterns are likely having a bigger impact on CMI than documentation and coding practices. As more services move to the outpatient setting, CMI increases because less acute patients are lowering the inpatient CMI.
What is case-mix adjustments?
Case-mix adjustment uses statistical models to predict what each hospital's ratings would have been for a standard patient or population, thereby removing from comparisons the predictable effects of differences in patient characteristics that are consistent across hospitals.
What is Medicare case mix index?
The Medicare case-mix index (CMI) reflects the costliness of a hospital's Medicare patient mix. The costs are based on the diagnosis-related group (DRG) in which each patient is classified and the weight that Medicare has applied to each DRG to reflect patients' relative costs. For Medicare patients for whom payment was made under the prospective payment system (PPS) in States not waived from the Medicare reimbursement system, the CMI for fiscal year 1984 was 9.2 percent higher than that for calendar year 1981. Because the calculatiorn; of budget neutrality that underlaid the PPS rates for 1984 assumed that the CMI would increase by only 3.4 percent, Medicare paid 5.6 percent more per PPS admission in that year than had been planned. 1 To guide the Health Care Financing Administration (HCFA) in how to deal with the unexpectedly large increase in the CMI, we undertook a study of the components of the increase. We sought to assess what part of the increase resulted from changes in coding practices, what part from changes in medical practices, and what part from changes in Medicare patients' resource needs.
What is the data base for Medicare enrollees?
Two major data bases on Medicare enrollees' inpatient episodes were used in this study: information from hospital bills that come to the Health Care Financing Administration (HCFA) through its intermediaries and discharge abstract data sent to the Commission on Professional and Hospital Activities (CPHA) from its subscriber hospitals. The latter data base is known as the Professional Activity Study
What Medicare files were used in 1981?
We used two different Medicare files for 1981 and 1984-85: MEOPAR and PATB1LL.2 We do not describe the MEDPAR file here, because it has been used extensively by researchers for some time (Pettengill and Vertrees, 1982.)
How many days does Medicare cover?
Medicare allows 90 covered benefit days for an episode of care under the inpatient hospital benefit. Each patient has an additional 60 lifetime reserve days. The patient may use these lifetime reserve days to cover additional non-covered days of an episode of care exceeding 90 days. High Cost Outlier.
How long does Medicare cover inpatient hospital care?
The inpatient hospital benefit covers 90 days of care per episode of illness with an additional 60-day lifetime reserve.
What is CMS case mix index?
Case Mix Index (CMI) is used by the Centers for Medicare and Medicaid Services (CMS) to determine funding allocation for Medicare and Medicaid beneficiaries in hospitals and other care facilities. Patients are classified into diagnosis-related groups (DRGs) depending on condition, case complexity, and medical needs.
What is the average CMI of a hospital?
The following tables list the top 25 hospitals with the largest case mix index. The average CMI of all 25 hospitals is 3.48, though CMIs range from 3.02 to 5.26.
