What makes a good Medicaid managed care plan?
Sep 09, 2020 · Medicare care managed care plans are an optional coverage choice for people with Medicare. Managed care plans take the place of your original Medicare coverage. Original Medicare is made up of Part...
What does managed care actually mean?
Jul 16, 2021 · Medicare managed care plans are an alternative to Original Medicare. Otherwise known as Medicare Advantage plans with many plan types, most are either HMOs or PPOs. Managed-care plans provide benefits for gaps in Parts A and B coverage. These alternative health-care plans make up Part C of Medicare.
How to apply for Medicaid Managed Care?
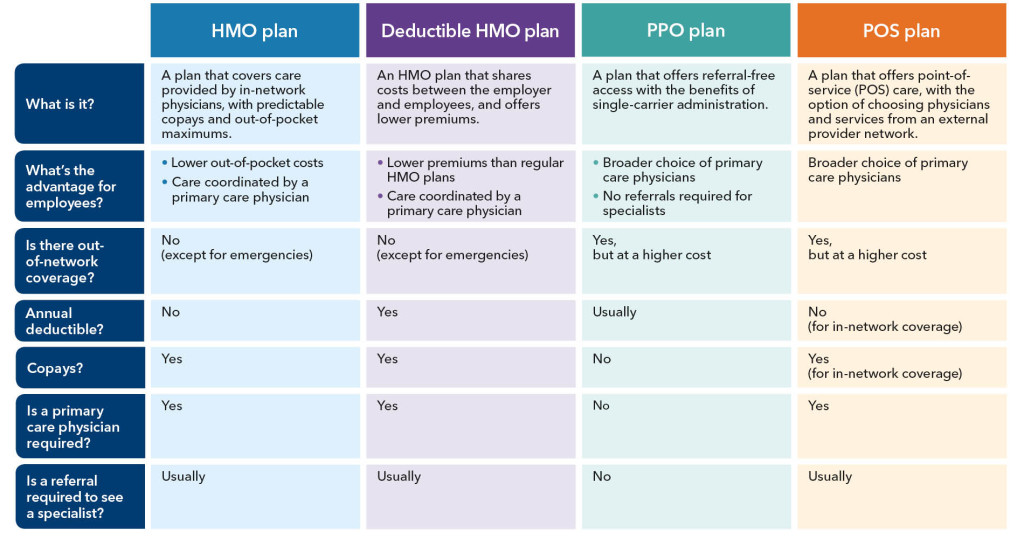
Nov 17, 2021 · A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) or POS (point of service) plans. These Medicare Advantage plans offer managed care that is coordinated between health care providers within a network.
What are the types of managed care?
Mar 01, 2022 · Medicare managed care is a type of government subsidized healthcare that functions as a health maintenance organization ( HMO ). Medicare is the insurance that the government provides to elderly people in the United States.

What is the difference between Medicare and Medicare managed care?
Medicare care managed care plans are an optional coverage choice for people with Medicare. Managed care plans take the place of your original Medicare coverage. Original Medicare is made up of Part A (hospital insurance) and Part B (medical insurance). Plans are offered by private companies overseen by Medicare.Sep 9, 2020
What is an example of a managed care plan?
A good example of a managed care plan is an HMO (Health Maintenance Organization). HMOs closely manage your care. Your cost is lowest with an HMO. You are limited to seeing providers in a small local network, which also helps keep costs low.
What is the difference between Medicare fee for service and Medicare managed care?
Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
What does managed care plan mean?
Managed care plans are a type of health insurance. They have contracts with health care providers and medical facilities to provide care for members at reduced costs. These providers make up the plan's network.Sep 20, 2018
What is the purpose of managed care?
The purpose of managed care is to enhance the quality of healthcare for all patient populations. Managed care revolves around the collaboration of health insurance plans and healthcare providers. Managed Care includes healthcare plans that are used to manage cost, utilization, and quality.Dec 29, 2020
How does managed care work?
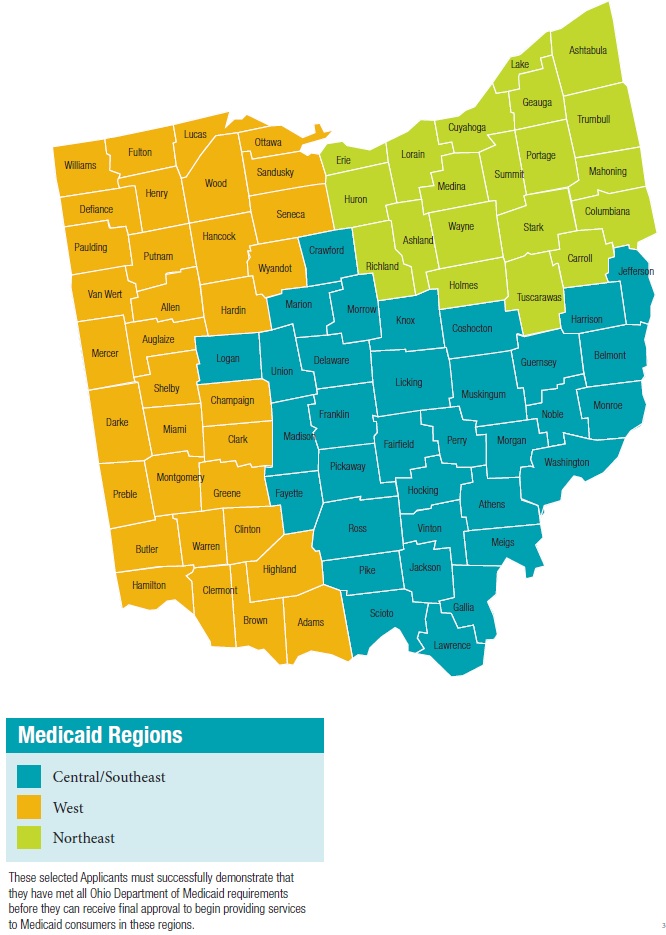
Under managed care, states sign contracts with "managed care organizations," or MCOs, that provide medical services through their own networks of doctors and hospitals. The state pays the MCO a fixed annual fee for each Medicaid patient. And the MCO takes responsibility for overseeing each person's care.May 31, 2011
What is the most common form of managed care?
HMOThe most common type of managed care plan is the HMO. If you enroll in an HMO plan, you'll need to pick a primary care provider who will direct all your healthcare needs and refer you to specialists when appropriate. You are only covered if you go to medical providers and facilities who are in your network.
What are the three main payment mechanisms used in managed care?
What are the three main payment mechanisms managed care uses? In each mechanism who bears the risk. The three main types of payment arrangements with providers are: capitation, discounted fees, and salaries.
Which part of Medicare is the managed care option?
Terms in this set (10) Which part of Medicare is the managed care option? Part C is Medicare's managed care option. Medicare Advantage is the name of the program.
What are the benefits of managed care?
What Are the Advantages of Managed Care?It lowers the costs of health care for those who have access. ... People can seek out care from within their network. ... Information moves rapidly within a network. ... It keeps families together. ... There is a certain guarantee of care within the network.More items...•Jun 14, 2017
What are two major differences between managed care and indemnity insurance?
Traditional Indemnity- insure pays a fixed monthly premium and 100% all bills till annual deductible then insurance pays up to maximum amount. Managed Care Plan- Pay monthly premiums, copays and sometimes deductible.
Which of the following is a disadvantage of managed care?
Benefits of managed care include patients having multiple options for coverage and paying lower costs for prescription drugs. Disadvantages include restrictions on where patients can get services and issues with finding referrals.Oct 20, 2018
What is Medicare Advantage 2021?
Updated on March 19, 2021. Medicare managed care plans are an alternative to Original Medicare. Otherwise known as Medicare Advantage plans with many plan types, most are either HMOs or PPOs. Managed-care plans provide benefits for gaps in Parts A and B coverage. These alternative health-care plans make up Part C of Medicare.
Why is it important to enroll in the right plan?
Enrolling in the right plan for you is key to making health-care more affordable. The number of Medicare beneficiaries enrolling in managed care plans is on the rise. Instead of working alongside Medicare-like Medigap insurance, Advantage plans replace Original Medicare. While providing additional benefits, these plans must also include all ...
What is indemnity health insurance?
Before HMOs, PPOs, and others, Indemnity plans were the main plans to choose from. Indemnity plans pre-determine the percentage of what they consider a reasonable and customary charge for certain services. Carriers pay a percentage of charges for a service and the member pays the remainder.
What are the benefits of Medicare managed care?
Benefits can include routine vision, dental and hearing services. Additionally, managed care plans offer prescription drug coverage. The cost of medications out-of-pocket can be financially exhausting. Medicare managed care plans can provide some relief.
What is managed care plan?
Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan. MA plans decide on rate amounts, making prices different from plan to plan. Processing payments are done through the private plan, not Medicare.
Is Medicare Supplement the same as Managed Care?
Managed-care plans and Medicare Supplement plans are not the same. This misconception is common. Both provide additional benefits to Original Medicare. However, they serve two totally different purposes. Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan.
Does an indemnity plan have a provider network?
Members will receive reimbursement for medical expenses (up to a certain amount). Indemnity plans have no provider network, members can visit the doctor (s) of their choice. Contrarily, managed care plans have a network (s) of providers, with different plan options.
What is a HMO plan?
Health maintenance organization (HMO) In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. Preferred provider organization (PPO)
What are the different types of Medicare plans?
Types of Medicare managed care plans 1 Health maintenance organization (HMO)#N#In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. 2 Preferred provider organization (PPO)#N#In a Medicare PPO plan, you may or may not use a primary care physician, and you are typically not required to get a referral to see a specialist. You’ll have a network of providers from which to choose .You will generally can receive at least some coverage when receiving care outside of the network of providers, though your health care services may cost more than if you received them from a provider within your plan network. 3 Point of service (POS)#N#You can use a primary care physician in a Point of Service plan, as you would with an HMO plan. But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
What is Medicare managed care?
A Medicare managed care plan is a type of Medicare Advantage plan. Learn what managed care plans are and how they could be a good fit for you. A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) ...
How to contact Medicare Advantage?
For more information about managed care plans or other types of Medicare Advantage plans, including plan benefits, eligibility, enrollment and availability, contact a licensed insurance agent by calling. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week.
Why do you see a primary care physician?
Seeing a primary care physician allows patients to build a rapport with their doctor, and the doctor gets to know the patient’s health history firsthand . When a patient is referred to a specialist, there is communication between the primary care physician and the specialist regarding the patient’s health and treatment.
Why are patient records transferred?
A patient’s medical records are typically transferred between providers in the network for increased communication. The increased coordination allows primary care physicians and other providers within the network to make more informed decisions regarding a beneficiary’s care.
What is managed care network?
The networks of managed care plans often include pharmacies, which can help make ordering and filling prescriptions faster and easier for everyone involved . There’s less uncertainty about a beneficiary’s costs for care in a managed care plan, provided they stay within the assigned network for qualified services.
When is the MA model enrollment period?
All enrollments with an effective date on or after January 1, 2021, must be processed in accordance with the revised guidance requirements, including the new model MA enrollment form. MA plans are expected to use the new model form for the 2021 plan year Annual Enrollment Period (AEP) which begins on October 15, 2020.
When does MA default enrollment start?
As outlined in the 2019 guidance, only MA organizations who meet the criteria outlined and are approved by CMS to conduct default enrollment for coverage effective dates of January 1, 2019 , or later.
What is post discharge reconciliation?
An MA plan may offer a post-discharge medication reconciliation as a supplemental benefit. For example, immediately following discharge (e.g., within the first week) from a hospital or SNF inpatient stay, MA plans may offer, as a supplemental benefit , the services of a qualified health care provider who, in cooperation with the enrollee’s physician, would review the enrollee’s complete medication regimen that was in place prior to admission and compare and reconcile with the regimen prescribed for the enrollee at discharge to ensure new prescriptions are obtained and discontinued medications are discarded. This reconciliation of the enrollee’s medications may be provided in the home and is designed to identify and eliminate medication side effects and interactions that could result in illness or injury.
What is a non-SNP physical exam?
Non-SNP MA plans may offer as a supplemental benefit a physical exam that provides services beyond those services required to be provided in the Annual Wellness Visit. To be considered an Annual Physical Exam that qualifies as a supplemental benefit by CMS, the exam would be provided by a qualified physician or qualified non-physician practitioner, hereafter referred to as a practitioner. At a minimum, the exam would include a detailed medical/family history and the performance of a detailed head to toe assessment with hands-on examination of all the body systems. For example, the practitioner uses visual inspection, palpation, auscultation and 133 manual examination in his/her full examination to assess overall general health and detect abnormalities or signs that could indicate a disease process that should be addressed. We consider these components minimum elements and not an exhaustive list.
What is general nutrition education?
General nutritional education for all enrollees through classes and/or individual counseling may be provided as a supplemental benefit as long as the services are provided by practitioners who are practicing in the state in which s/he is licensed or certified, and are furnishing services within the scope of practice defined by their licensing or certifying state. (i.e., physician, nurse, registered dietician or nutritionist). The number of visits, time limitations, and whether the benefit is for classes and/or individual counseling must be defined in the PBP.
What is Medicare Part B?
Medicare Part B covers individual and group therapy services to diagnose and treat mental illness. The Part B coverage usually requires a physician referral for mental health care and is based on a mental health diagnosis.
Is POS a mandatory benefit?
HMOs may offer a POS option as a mandatory or optional supplemental benefit pursuant to 42 CFR 422.105 and 422.111. This supplemental benefit may not be offered by any other MA plan type. The POS benefit provides coverage for some plan-covered services outside of the HMO’s network. The HMO plan:
Does MA offer chiropractic care?
MA plans may choose to offer routine chiropractic services as a supplemental benefit as long as the services are provided by a state-licensed chiropractor practicing in the state in which he/she is licensed and is furnishing services within the scope of practice defined by that state’s licensure and practice guidelines. The routine services may include conservative management of neuromusculoskeletal disorders and related functional clinical conditions including, but not limited to, back pain, neck pain and headaches, and the provision of spinal and other therapeutic manipulation/adjustments.
Does MA offer alternative therapies?
MA plans may offer alternative therapies as supplemental benefits. These alternative therapies must be provided by practitioners who are licensed or certified, as applicable, in the state in which they practice and are furnishing services within the scope of practice defined by their licensing or certifying state. MA plans are to provide a description of therapies offered in the PBP Notes section.
Medicare Vs Medicaid: Whats The Difference
Understand the differences between Medicare and Medicaid and find out if you can qualify for both.
Types Of Medicare Managed Care Plans
Moreover, care plans are private health insurance companies that Medicare-approves. Plans offer care from a specific network of providers at a lower overall cost. Medicare divides managed care plans into different plan types. Classifying each by using acronyms such as HMO, PFFS, PPO, or HMO-POS.
Opting For Part A Only
Some people choose only to have Medicare Part A coverage so that they dont have to pay the monthly premiums for Medicare Parts B and D. If you still have insurance through a current employer , you can add the other parts later with no penalty.
How The Programs Differ
Medicare is an insurance program while Medicaid is a social welfare program.
How Can I Find Which Medicare Advantage Plans Are Available In My Area
Im available to help you understand your options. If you prefer, you can request information via email or schedule a phone call at your convenience by clicking one of the links below. To view some plans you may be eligible for, use the Compare Plans button below.
Medicare Advantage Managed Care Plans: Beneficiary Protections
The plan cannot charge more than a $50 copayment for visits to the emergency room.
Medicare Advantage Plans May Cost You Less
If you enroll in a Medicare Advantage plan, you continue to pay your Medicare Part B premium and you may pay an additional premium. The insurer determines the Medicare Advantage plans premium, which can vary from one Medicare Advantage plan to another. Some Medicare Advantage plans may have premiums as low as $0.
What is HMO insurance?
Health Maintenance Organization (HMO) manages care by requiring you to see network providers, usually for a much lower monthly premium. HMOs also often require you to see a PCP before going elsewhere, and do not cover you to see providers outside the network. Preventive care is covered at 100%.
What is no cost preventive care?
No-cost preventive care is a big incentive for plan members to try and maintain good health. Primary Care Providers (PCP): Your health plan may require you to choose a PCP if you don’t already have one. You may be required to see your PCP first before going to any other doctor or specialist.
What is preventive care incentive?
Preventive care incentives: Managed care plans typically focus on making preventive care a priority. Most preventive services, such as annual check-ups, routine screenings, and certain vaccines, are covered at 100% by your health plan.
What are some examples of managed care?
They are examples of managed care: Provider networks: Health insurance companies contract with groups of providers to offer plan members reduced rates on care and services. These networks can include doctors, specialists, hospitals, labs, and other health care facilities. Some health plans require you to use the plan’s provider network ...
How does managed care work?
The primary way in which managed care plans work is by establishing provider networks. A provider network serves plan members over a certain geographic area in which the health plan is available. The providers in these networks agree to offer their services at reduced costs. Your health plan pays more of the cost of your care if you see providers ...
What is managed care organization?
A managed care organization or MCO is a health care company or a health plan that is focused on managed care as a model to limit costs, while keeping quality of care high.
What is a prior authorization?
Prior authorization: Most managed care plans require you to get approval before you have certain types of procedures or treatments done, or are prescribed certain types of specialty medications. This is called prior authorization, precertification, or preapproval, depending on your insurer. Part of managed care’s goal is to help ensure you are not ...