What you should know about Medicare Part D?
Main article: Medicare Part D The MMA's most touted feature is the introduction of an entitlement benefit for prescription drugs, through tax breaks and subsidies. In the years since Medicare's creation in 1965, the role of prescription drugs …
Is Medicare Part D Worth It?
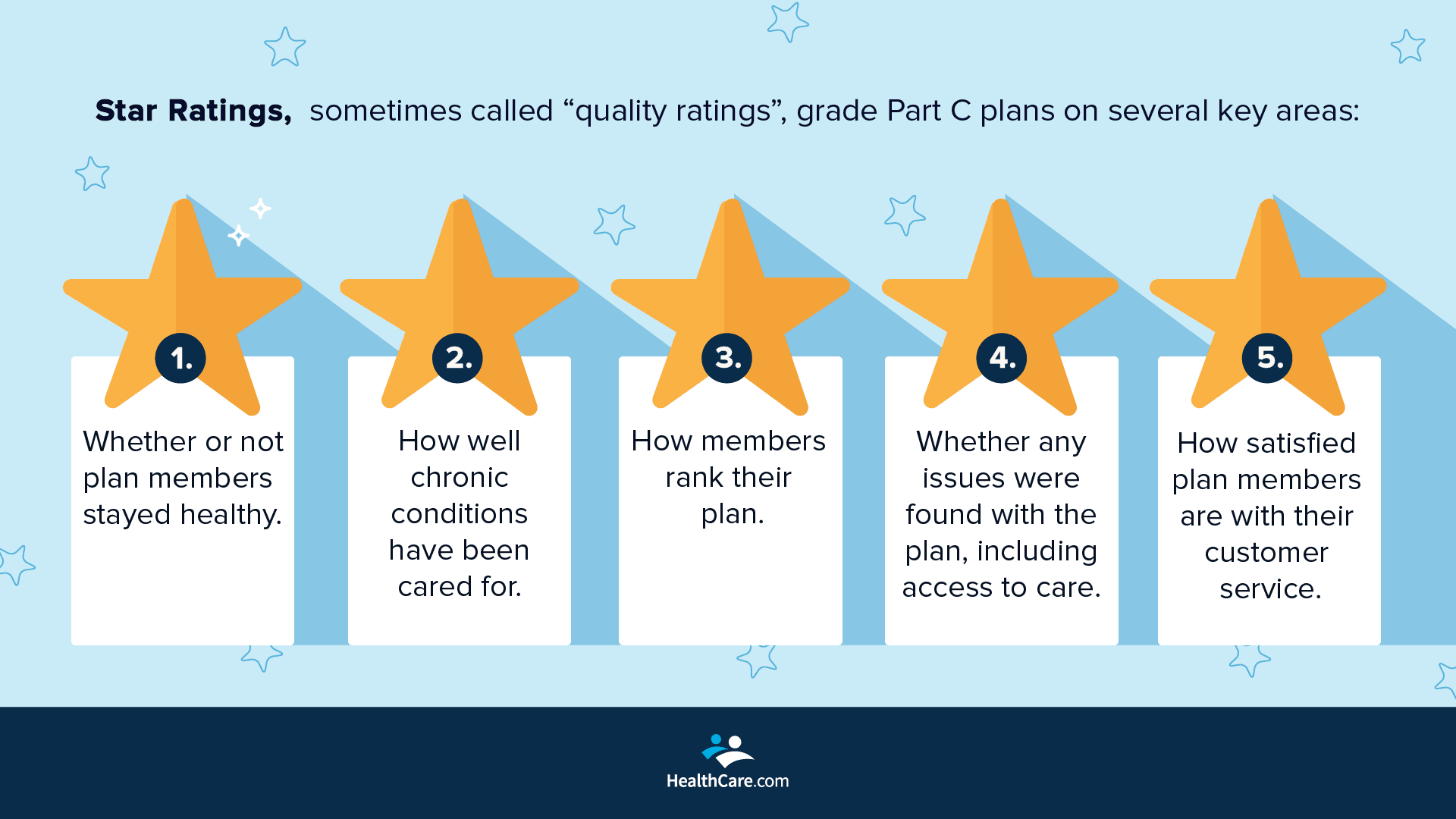
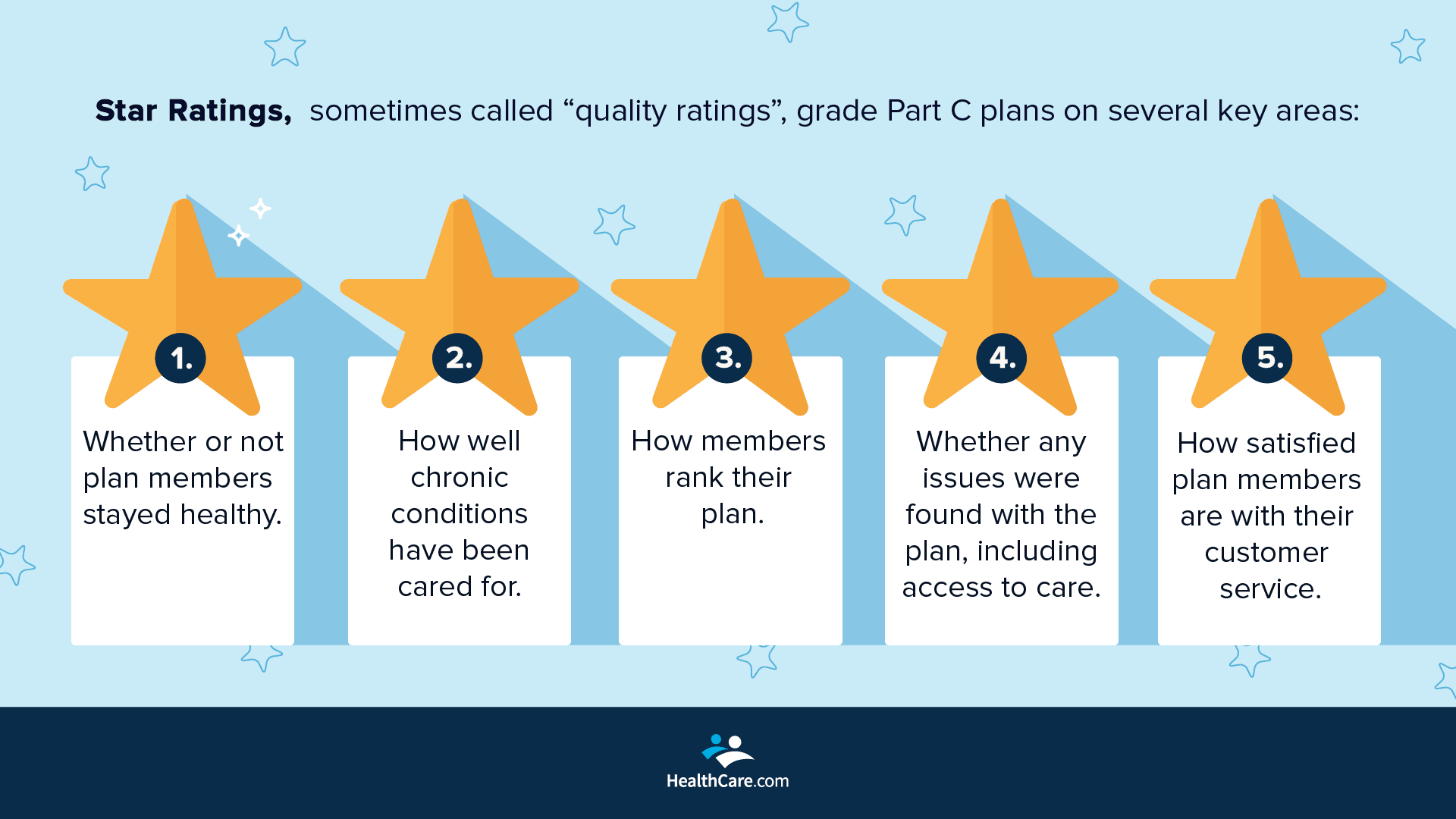
Medicare Advantage is a type of health insurance plan in the United States that provides Medicare benefits through a private-sector health insurer. In a Medicare Advantage plan, a Medicare beneficiary pays the Medicare monthly premium to the federal government, but receives coverage via a private insurance company for inpatient hospital and outpatient services. …
What does Medicare Part D really cost?
Apr 07, 2022 · Medicare Advantage enrollees must still pay the Part B premium. Part D is the prescription drug benefit, funded by general revenue and beneficiary premiums. Part D benefits can be obtained in two ways: either (1) purchased on a stand-alone basis, or (2) when combined with Part C. Table 1 shows the various coverage options. Health savings account
What are the best Medicare Part D plans?
Part D (Drug coverage): Helps cover the cost of prescription drugs (including many recommended shots or vaccines). You join a Medicare drug plan in addition to Original Medicare , or you get it by joining a Medicare Advantage Plan with drug coverage. Plans that offer Medicare drug coverage are run by private insurance companies that follow rules set by Medicare.

What is Medicare Part D?
Medicare Part D, the prescription drug benefit, is the part of Medicare that covers most outpatient prescription drugs. Part D is offered through private companies either as a stand-alone plan, for those enrolled in Original Medicare, or as a set of benefits included with your Medicare Advantage Plan.
What is the main problem with Medicare Part D?
The real problem with Medicare Part D plans is that they weren't set up with the intent of benefiting seniors. They were set up to benefit: –Pharmacies, by having copays for generic medications that are often far more than the actual cost of most of the medications.
What is the difference between Part B and Part D drugs?
Medicare Part B only covers certain medications for some health conditions, while Part D offers a wider range of prescription coverage. Part B drugs are often administered by a health care provider (i.e. vaccines, injections, infusions, nebulizers, etc.), or through medical equipment at home.Oct 1, 2021
What's the difference between Medicare Part C and D?
Medicare part C is called "Medicare Advantage" and gives you additional coverage. Part D gives you prescription drug coverage.
What is the most popular Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
What does Medicare D cost?
The national base beneficiary premium for Part D plans is $33.37 per month for 2022, according to the Centers for Medicare & Medicaid Services, which calculates this number in part by using the national average monthly bid amount submitted by private insurers.
Is Medicare Part D deducted from Social Security?
You can have your Part C or Part D plan premiums deducted from Social Security. You'll need to contact the company that sells your plan to set it up. It might take several months to set up and for automatic payments to begin.Dec 1, 2021
Which service is covered by Medicare Part D but not B or A?
You must have either Part A or Part B to be eligible for Part D. Part D is only available through private companies. Part B is the Medicare outpatient benefit. It covers most doctor's services, durable medical equipment, preventive care, ambulance services, and more.
What is the difference between Medicare B and Medicare D?
What is the difference between Medicare Part B and Medicare Part D? Medicare Part B covers costs relating to the diagnosis and treatment of medical conditions. Medicare Part D covers prescription drugs. Specific rules usually apply to both.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Can you have both Medicare Part C and D?
Can you have both Medicare Part C and Part D? You can't have both parts C and D. If you have a Medicare Advantage plan (Part C) that includes prescription drug coverage and you join a Medicare prescription drug plan (Part D), you'll be unenrolled from Part C and sent back to original Medicare.
What are the 4 phases of Medicare Part D coverage?
If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage. Select a stage to learn more about the differences between them.Oct 1, 2021
What is CMS in healthcare?
The Centers for Medicare and Medicaid Services (CMS), a component of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children's Health Insurance Program (CHIP), the Clinical Laboratory Improvement Amendments (CLIA), and parts of the Affordable Care Act (ACA) ("Obamacare").
How much does Medicare cost in 2020?
In 2020, US federal government spending on Medicare was $776.2 billion.
What is Medicare and Medicaid?
Medicare is a national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, ...
How is Medicare funded?
Medicare is funded by a combination of a specific payroll tax, beneficiary premiums, and surtaxes from beneficiaries, co-pays and deductibles, and general U.S. Treasury revenue. Medicare is divided into four Parts: A, B, C and D.
What is a RUC in medical?
The Specialty Society Relative Value Scale Update Committee (or Relative Value Update Committee; RUC), composed of physicians associated with the American Medical Association, advises the government about pay standards for Medicare patient procedures performed by doctors and other professionals under Medicare Part B.
How many people have Medicare?
In 2018, according to the 2019 Medicare Trustees Report, Medicare provided health insurance for over 59.9 million individuals —more than 52 million people aged 65 and older and about 8 million younger people.
When did Medicare Part D start?
Medicare Part D went into effect on January 1, 2006. Anyone with Part A or B is eligible for Part D, which covers mostly self-administered drugs. It was made possible by the passage of the Medicare Modernization Act of 2003. To receive this benefit, a person with Medicare must enroll in a stand-alone Prescription Drug Plan (PDP) or public Part C health plan with integrated prescription drug coverage (MA-PD). These plans are approved and regulated by the Medicare program, but are actually designed and administered by various sponsors including charities, integrated health delivery systems, unions and health insurance companies; almost all these sponsors in turn use pharmacy benefit managers in the same way as they are used by sponsors of health insurance for those not on Medicare. Unlike Original Medicare (Part A and B), Part D coverage is not standardized (though it is highly regulated by the Centers for Medicare and Medicaid Services). Plans choose which drugs they wish to cover (but must cover at least two drugs in 148 different categories and cover all or "substantially all" drugs in the following protected classes of drugs: anti-cancer; anti-psychotic; anti-convulsant, anti-depressants, immuno-suppressant, and HIV and AIDS drugs). The plans can also specify with CMS approval at what level (or tier) they wish to cover it, and are encouraged to use step therapy. Some drugs are excluded from coverage altogether and Part D plans that cover excluded drugs are not allowed to pass those costs on to Medicare, and plans are required to repay CMS if they are found to have billed Medicare in these cases.
What is LIS in Medicare?
The Low-Income Subsidy (LIS), also known as "Extra Help" provides additional cost-sharing and premium assistance for eligible low-income Medicare Part D beneficiaries with incomes below 150% the Federal Poverty Level and limited assets. Individuals who qualify for the Low-Income Subsidy (LIS) or who are also enrolled in Medicaid do not have a coverage gap.
How much does Medicare pay for a donut hole?
Medicare Part D beneficiaries who reach the Donut Hole will also pay a maximum of 25% co-pay on generic drugs purchased while in the Coverage Gap (receiving a 75% discount). For example: If you reach the 2020 Donut Hole, and your generic medication has a retail cost of $100, you will pay $25. The $25 that you spend will count toward your TrOOP ...
What is Medicare Part D coverage gap?
Period of consumer payment for prescription medication costs. The Medicare Part D coverage gap (informally known as the Medicare doughnut hole) is a period of consumer payment for prescription medication costs which lies between the initial coverage limit and the catastrophic-coverage threshold, when the consumer is a member ...
How much is Medicare Part D 2020?
The 2020 Medicare Part D standard benefit includes a deductible of $435 (amount beneficiaries pay out of pocket before insurance benefits kick in) and 25% co-insurance, up to $6,350.
What percentage of Medicare Part D enrollees in 2007 were not eligible for low income subsidies?
The most common forms of gap coverage cover generic drugs only. Among Medicare Part D enrollees in 2007 who were not eligible for the low-income subsidies, 26 percent had spending high enough to reach the coverage gap. Fifteen percent of those reaching the coverage gap (four percent overall) had spending high enough to reach ...
What is the gap between insurance and consumer?
The gap is reached after shared insurer payment - consumer payment for all covered prescription drugs reaches a government-set amount, and is left only after the consumer has paid full, unshared costs of an additional amount for the same prescriptions.
When will the Medicare doughnut hole close?
From 2017 to 2020, brand-name drug manufacturers and the federal government will be responsible for providing subsidies to patients in the doughnut hole.
What is Medicare Part D?
Main article: Medicare Part D. The MMA's most touted feature is the introduction of an entitlement benefit for prescription drugs, through tax breaks and subsidies. In the years since Medicare's creation in 1965, the role of prescription drugs in patient care has significantly increased.
What is the "donut hole" in Medicare?
The "donut hole" provision of the Patient Protection and Affordable Care Act was an attempt to correct the issue.
When was Medicare Modernization Act enacted?
Signed into law by President George W. Bush on December 8, 2003. The Medicare Prescription Drug, Improvement, and Modernization Act, also called the Medicare Modernization Act or MMA, is a federal law of the United States, enacted in 2003. It produced the largest overhaul of Medicare in the public health program's 38-year history.
How many Americans were enrolled in HSAs in the first 10 years?
After the first 10 years over 12 million Americans were enrolled in HSAs (AHIP;EBRI).
How much did the stimulus program cost in 2015?
One month after passage, the administration estimated that the net cost of the program over the period between 2006 (the first year the program started paying benefits) and 2015 would be $534 billion. As of February 2009, the projected net cost of the program over the 2006 to 2015 period was $549.2 billion.
Can Medicare negotiate drug prices?
Since the enactment of Medicare Prescription Drug, Improvement, and Modernization Act in 2003, only insurance companies administering Medicare prescription drug program, not Medicare, have the legal right to negotiate drug prices directly from drug manufacturers.
When did Medicare Advantage start?
Medicare Advantage plans. With the passage of the Balanced Budget Act of 1997, Medicare beneficiaries were given the option to receive their Medicare benefits through private health insurance plans, instead of through the Original Medicare plan (Parts A and B).
What is the difference between Medicare Advantage and Original Medicare?
From a beneficiary's point of view, there are several key differences between Medicare Advantage and Original Medicare. Most Medicare Advantage plans are managed care plans (e.g., PPOs or HMOs) with limited provider networks, whereas virtually every physician and hospital in the U.S. accepts Original Medicare.
What is Medicare Advantage?
Medicare Advantage (sometimes called Medicare Part C or MA) is a type of health insurance plan in the United States that provides Medicare benefits through a private-sector health insurer. In a Medicare Advantage plan, a Medicare beneficiary pays a monthly premium to a private insurance company ...
What happens if Medicare bid is lower than benchmark?
If the bid is lower than the benchmark, the plan and Medicare share the difference between the bid and the benchmark ; the plan's share of this amount is known as a "rebate," which must be used by the plan's sponsor to provide additional benefits or reduced costs to enrollees.
How does capitation work for Medicare Advantage?
For each person who chooses to enroll in a Part C Medicare Advantage or other Part C plan, Medicare pays the health plan sponsor a set amount every month ("capitation"). The capitated fee associated with a Medicare Advantage and other Part C plan is specific to each county in the United States and is primarily driven by a government-administered benchmark/framework/competitive-bidding process that uses that county's average per-beneficiary FFS costs from a previous year as a starting point to determine the benchmark. The fee is then adjusted up or down based on the beneficiary's personal health condition; the intent of this adjustment is that the payments be spending neutral (lower for relatively healthy plan members and higher for those who are not so healthy).
How many people will be on Medicare Advantage in 2020?
Enrollment in the public Part C health plan program, including plans called Medicare Advantage since the 2005 marketing period, grew from zero in 1997 (not counting the pre-Part C demonstration projects) to over 24 million projected in 2020. That 20,000,000-plus represents about 35%-40% of the people on Medicare.
How much does Medicare pay in 2020?
In 2020, about 40% of Medicare beneficiaries were covered under Medicare Advantage plans. Nearly all Medicare beneficiaries (99%) will have access to at least one Medicare Advantage ...
How much has Medicare Advantage decreased since 2017?
Since 2017, the average monthly Medicare Advantage premium has decreased by an estimated 27.9 percent. This is the lowest that the average monthly premium for a Medicare Advantage plan has been since 2007 right after the second year of the benchmark/framework/competitive-bidding process.
How many PDPs are there in Medicare?
PDPs are avaialble everwhere and in large numbers. All Medicare beneficiaries have access to between 40 and 60 PDPs). Like MA benefits, PDP benefits are also highly subsidized by Medicare. Medicare pays approximately 75% of the value of coverage, the beneficiary pays the remaining 25%.
How is Medicare funded?
Medicare is organized in four parts: Part A is hospital insurance, funded by a 2.9% payroll tax (shared equally between employer and employee). Part B is outpatient coverage, funded by premiums and general revenue. Part C is the Medicare Advantage program, under which private insurers bundle Parts A, B, and in some cases D, ...
What is wrap around coverage?
Wrap around coverage. Either through an employer or the non-group market, some beneficiaries obtain additional wrap around coverage, known as Medigap. Medigap plans are standardized in most states (MA, WI, MN are exceptions) and cover cost sharing and other benefits not covered by Medicare.
What is Medicare insurance?
Medicare. From Bogleheads. Jump to navigation Jump to search. Medicare is a federal public health insurance program for the elderly and qualified disabled. It is a financing program not a health delivery system. It relies on private health providers to deliver health care to program beneficiaries.
When was Medicare established?
Brief overview and history. Medicare was established in 1965 under Title XVIII of the Social Security Act to provide health insurance for elderly Americans. Prior to Medicare, nearly half the elderly lacked health insurance. Today, health insurance for the elderly is nearly universal. Medicare was expanded in 1972 to provide health insurance ...
Is Medicare Advantage a private insurance?
Medicare Advantage. Health maintenance organizations (HMOs) offered by private insurers have existed under Medicare since the 1970s. Medicare now contracts with a variety of types of private plans: preferred provider organizations (PPOs), provider-sponsored organizations (PSOs), private fee-for-service (PFFS) plans.
Does Medicare cover MA?
That is, it costs Medicare more for a beneficiary to enroll in an MA plan then it would for Medicare to cover that beneficiary directly. Not all MA plan types are available everywhere. Historically, MA plans have been concentrated in urban regions. In the past some rural counties had no MA offerings.
What is a Medigap policy?
Medigap policy with creditable drug coverage. Prescription drug coverage (for example, from an employer or union) that's expected to pay, on average, at least as much as Medicare's standard prescription drug coverage.
Do you have to pay late enrollment penalty for Medigap?
You'll probably have to pay a late enrollment penalty if you have a Medigap policy that doesn't include creditable prescription drug coverage and you decide to join a Medicare Prescription Drug Plan later. This means you'll pay a higher monthly premium than if you joined when you were first eligible.
Does Medigap have to send a notice?
Your Medigap company must send you a notice each year telling you if the prescription drug coverage in your Medigap policy is creditable. Keep these notices in case you decide later to join a Medicare drug plan.
Can you get your Medicare coverage back if you have a Medigap policy?
If your Medigap policy covers prescription drugs, you'll need to tell your Medigap insurance company if you join a Medicare Prescription Drug Plan. The Medigap insurance company will remove the prescription drug coverage from your Medigap policy and adjust your premium. Once the drug coverage is removed, you can't get that coverage back, even though you didn't change Medigap policies.
What are the benefits of Medicare Advantage Plan?
Additional benefits that many Medicare Advantage plans include are: Vision coverage. Hearing coverage. Dental coverage. Medicare Part D prescription drug coverage. If you’re eligible for Medicare Part A and Part B, and do not have ESRD, you can join a Medicare Advantage Plan. Medicare beneficiaries have the option of receiving health care benefits ...
What is Medicare Advantage?
Medicare Advantage (Part C) is an alternative to Original Medicare. It allows you to receive Part A and Part B benefits — and in many cases, other benefits — from a private health insurance plan. At the very least, your Medicare Advantage plan must offer the same benefits as Original Medicare. The only exception is hospice care, which is still ...
How long do you have to be on Medicare if you are 65?
For those younger than 65, you are only eligible to receive Medicare benefits if you: Have received Social Security or Railroad Retirement Board (RRB) disability benefits for 24 months.
How many parts are there in Medicare?
There are four different parts of Medicare: Part A, Part B, Part C, and Part D — each part covering different services. Understanding how these parts and services work (together and separately) is the key to determining which ones fit your unique health care needs and budget. There are two main paths for Medicare coverage — enrolling in Original ...
When do you get Medicare for ALS?
If you’re under 65, it’s the 25th month you receive disability benefits. ALS patients are automatically enrolled in Medicare coverage when their Social Security disability benefits begin, regardless of age. If you have end-stage renal disease (ESRD), you must manually enroll.
Does Medicare Advantage include Part D?
Many Medicare Advantage plans also include Part D coverage. If you're looking for Medicare prescription drug coverage, you can consider enrolling in a Medicare Advantage plan that includes drug coverage, or you can consider enrolling in a Medicare Part D plan. You can compare Part D plans available where you live and enroll in a Medicare ...
When do you get a disability if you are 65?
If you’re under 65, it’s the 25th month you receive disability benefits.
What is IRMAA Part D?
For Part D, the IRMAA amounts are added to the regular premium for the enrollee’s plan (Part D plans have varying prices, so the full amount, after the IRMAA surcharge, will depend on the plan).
What is the Medicare surcharge for 2021?
This means that for your 2021 Medicare premiums, your 2019 income tax return is used. This amount is recalculated annually. The IRMAA surcharge will be added to your 2021 premiums if your 2019 income was over $88,000 (or $176,000 if you’re married), but as discussed below, there’s an appeals process if your financial situation has changed.
How is IRMAA determined?
IRMAA is determined by income from your income tax returns two years prior. How IRMAA affects Part B premiums depends on your household income. IRMAA surcharges are added to you Part D premiums. You can appeal your IRMAA determination if you believe the calculation was erroneous. The SECURE Act of 2019 could further affect your premiums.
What is IRMAA in Social Security?
The income used to determine IRMAA is a form of Modified Adjusted Gross Income (MAGI), but it’s specific to Medicare.
What is IRMAA Medicare?
What is IRMAA? For Medicare beneficiaries who earn over $88,000 a year – and who are enrolled in Medicare Part B and/or Medicare Part D – it’s important to understand the income-related monthly adjusted amount (IRMAA), which is a surcharge added to the Part B and Part D premiums.
What age can you contribute to an IRA?
The SECURE Act has a number of different features – such as allowing IRA contributions after age 70½ if you’re still earning an income – and it extends the minimum age that one must receive RMDs (Required Minimum Distributions) from 70½ to 72. Note that those who are already at least 70½ must continue to receive RMDs.
Does delaying RMDs reduce IRMAA?
The reason this may be important is that it is possible that delaying receiving RMDs may also reduce IRMAA if your Modified Adjusted Gross Income is close to the limits stated in the Tables 1 and 2.
Overview
Medicare is a government national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disabilitystatus as determined by the SSA, includ…
History
Originally, the name "Medicare" in the United States referred to a program providing medical care for families of people serving in the military as part of the Dependents' Medical Care Act, which was passed in 1956. President Dwight D. Eisenhowerheld the first White House Conference on Aging in January 1961, in which creating a health care program for social security beneficiaries was p…
Administration
The Centers for Medicare and Medicaid Services (CMS), a component of the U.S. Department of Health and Human Services (HHS), administers Medicare, Medicaid, the Children's Health Insurance Program (CHIP), the Clinical Laboratory Improvement Amendments (CLIA), and parts of the Affordable Care Act (ACA) ("Obamacare"). Along with the Departments of Labor and Treasury, the CMS also implements the insurance reform provisions of the Health Insurance Portability an…
Financing
Medicare has several sources of financing.
Part A's inpatient admitted hospital and skilled nursing coverage is largely funded by revenue from a 2.9% payroll taxlevied on employers and workers (each pay 1.45%). Until December 31, 1993, the law provided a maximum amount of compensation on which the Medicare tax could be imposed annually, in the same way that the Social Security payroll tax operates. Beginning on January 1, …
Eligibility
In general, all persons 65 years of age or older who have been legal residents of the United States for at least five years are eligible for Medicare. People with disabilities under 65 may also be eligible if they receive Social Security Disability Insurance (SSDI) benefits. Specific medical conditions may also help people become eligible to enroll in Medicare.
People qualify for Medicare coverage, and Medicare Part A premiums are entirely waived, if the f…
Benefits and parts
Medicare has four parts: loosely speaking Part A is Hospital Insurance. Part B is Medical Services Insurance. Medicare Part D covers many prescription drugs, though some are covered by Part B. In general, the distinction is based on whether or not the drugs are self-administered but even this distinction is not total. Public Part C Medicare health plans, the most popular of which are bran…
Out-of-pocket costs
No part of Medicare pays for all of a beneficiary's covered medical costs and many costs and services are not covered at all. The program contains premiums, deductibles and coinsurance, which the covered individual must pay out-of-pocket. A study published by the Kaiser Family Foundation in 2008 found the Fee-for-Service Medicare benefit package was less generous than either the typical large employer preferred provider organization plan or the Federal Employees He…
Payment for services
Medicare contracts with regional insurance companies to process over one billion fee-for-service claims per year. In 2008, Medicare accounted for 13% ($386 billion) of the federal budget. In 2016 it is projected to account for close to 15% ($683 billion) of the total expenditures. For the decade 2010–2019 Medicare is projected to cost 6.4 trillion dollars.
For institutional care, such as hospital and nursing home care, Medicare uses prospective payme…