The Centers for Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Full Answer
What does provider status mean for pharmacists?
Provider status would align reimbursement with the services pharmacists are trained to provide and give underserved patients more access to crucial care. and be reimbursed at 85% of the physician fee schedule.
What's the difference between a preferred and standard pharmacy?
One way you may be able to save is by using a preferred pharmacy instead of a standard pharmacy. What's the difference between preferred and standard? A preferred pharmacy offers a lower copay for covered drugs than a standard pharmacy. Take a look at what you can save with this example, based on our 2022 BCN Advantage SM HMO-POS Classic plan.
Should pharmacists be eligible for Medicare Part B provider status?
If they are granted Medicare Part B provider status, more pharmacists would be authorized to provide patients with an expanded set of services, reducing the current burden on other sites of care.
What do I need to know about Medicare prescription drug coverage?
Things to know. Drugs that aren't covered under Part B may be covered under Medicare prescription drug coverage (Part D). If you have Part D coverage, check your plan's Formulary to see what outpatient prescription drugs the plan covers.
Why is it important for pharmacists to bill for patient care services under Medicare Part B?
Why are pharmacists considered providers?
What is the Pharmacy and Medically Underserved Areas Enhancement Act?
What is the top priority for pharmacy?
Can a pharmacist bill Medicare?
See more
About this website
What does standard pharmacy mean?
The Centers for Medicare and Medicaid (CMS) defines a non-preferred or standard network pharmacy as: "A pharmacy that's part of a Medicare drug plan's [pharmacy] network, but isn't a preferred pharmacy.
What is the difference between a preferred and a standard pharmacy?
Preferred in-network pharmacy: most often offer prescriptions at lowest cost-sharing amount. Standard in-network pharmacy: typically, prescriptions will have a higher cost-sharing amount. Out of network pharmacy: at an out of network pharmacy you will not be able to utilize your prescription drug coverage.
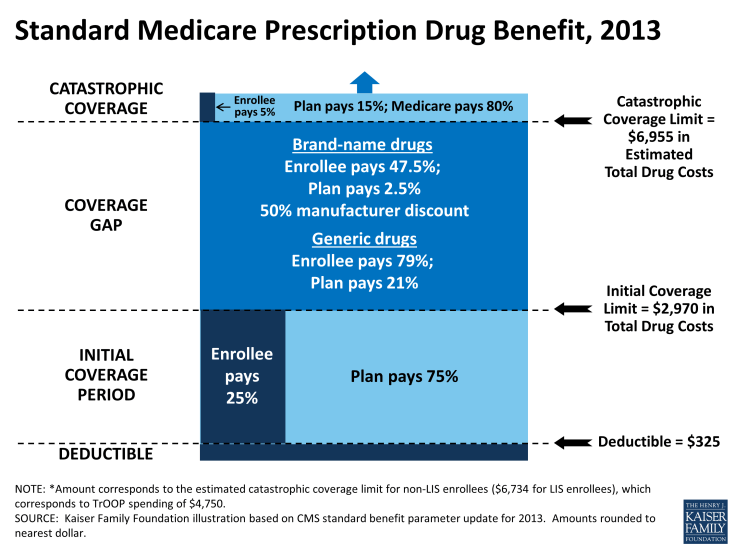
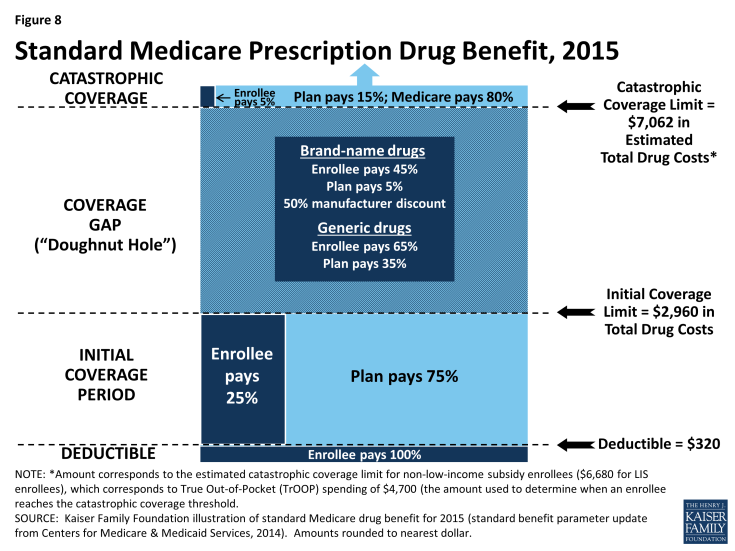
What are the 4 standardized levels of Medicare prescription drug coverage?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
What does standard cost sharing pharmacy mean?
Preferred cost sharing is a term that refers to lower out-of-pocket costs (often reduced co-pays) for prescription drugs when a beneficiary uses a designated subset of pharmacies in the network.
Is Walgreens a Medicare preferred pharmacy?
Walgreens will continue to be a part of preferred pharmacy networks with three national Medicare Part D plan sponsors: Humana. UnitedHealthcare.
What makes a pharmacy a preferred pharmacy?
In the United States, a preferred pharmacy network is a group of pharmacies that involves a prescription drug plan that selects a group of preferred pharmacies, which likely include pharmacies willing to give the plans a larger discount than other pharmacies.
What are Tier 1 Tier 2 and Tier 3 drugs?
Level or Tier 1: Low-cost generic and brand-name drugs. Level or Tier 2: Higher-cost generic and brand-name drugs. Level or Tier 3: High-cost, mostly brand-name drugs that may have generic or brand-name alternatives in Levels 1 or 2. Level or Tier 4: Highest-cost, mostly brand-name drugs.
What is the max out of pocket for Medicare Part D?
As expected, a $2,000 cap on out-of-pocket spending would generate larger savings than a $3,100 cap. Average out-of-pocket spending was $3,216 among the 1.2 million Part D enrollees with out-of-pocket spending above $2,000 in 2019.
Is Medicare going to do away with the donut hole?
The Part D coverage gap (or "donut hole") officially closed in 2020, but that doesn't mean people won't pay anything once they pass the Initial Coverage Period spending threshold. See what your clients, the drug plans, and government will pay in each spending phase of Part D.
What is the difference between preferred cost sharing and standard cost sharing?
What is the difference between a preferred cost-share and standard cost-share pharmacy? Answer: Preferred cost-share pharmacies may provide prescriptions for our Medicare members at a lower cost (for example, copayments) than standard in-network cost-share pharmacies, depending on the plan.
What does non preferred pharmacy mean?
The Centers for Medicare and Medicaid (CMS) defines a non-preferred or standard network pharmacy as: "A pharmacy that's part of a Medicare drug plan's [pharmacy] network, but isn't a preferred pharmacy.
Why do insurance companies have preferred pharmacies?
Insurers can create preferred pharmacy networks via selective contracts. The use of preferred pharmacy networks helps nudge policyholders toward locations with lower out-of-pocket costs and increases insurers' bargaining leverage with pharmacies, which can lower the overall price of their members' prescriptions.
Pharmacist "Incident To" E/M | Medical Billing and Coding Forum - AAPC
If this is your first visit, be sure to check out the FAQ & read the forum rules.To view all forums, post or create a new thread, you must be an AAPC Member.If you are a member and have already registered for member area and forum access, you can log in by clicking here.If you've forgotten your username or password use our password reminder tool.
Provider Status in the States - Pharmacy Times
State pharmacy associations are working to advance provider status legislation at the state and federal levels. With the introduction of House of Representatives Bill 4190, attention to pharmacist provider status at both the federal and state levels has greatly increased in the pharmacy community.
Provider Status for Pharmacists: It’s About Time
During American Pharmacists Month, and as the country uses all available health care resources to address COVID-19, there has never been a better or more important time to grant provider status to pharmacists.
What is the status of a pharmacy?
The status of a pharmacy is dependent upon the contract the prescription drug plan (Part D) has with the pharmacy. Individual Part D plans can place a pharmacy (physical or mail-order) in 1 of 3 categories: Preferred pharmacies will have the lowest copays and coinsurance, typically providing you with the most savings.
How often does Part D change?
Also note that a Part D plan’s network can (and usually does) change every calendar year as contracts renew or terminate. Copays, coinsurance, monthly premiums, and the Tier of a medication also change every year. So, make sure you review your plan every year, but let us do the hard work for you!
Can you pay 100% of the cost of a prescription at an out-of-network pharmacy?
Out-of-Network pharmacies want to be avoided if possible as you will pay 100% of the cost. In some rare cases, the price of a medication may be cheaper at a standard pharmacy. But, this will ONLY occur if the retail price is cheaper than the copay of the medication.
Why is it important for pharmacists to bill for patient care services under Medicare Part B?
Use these Quick Facts to explain how authorizing pharmacists to bill for patient care services under Medicare Part B improves access to health care and improves outcomes in underserved communities.
Why are pharmacists considered providers?
Evidence shows that pharmacists make a significant impact on patients’ health outcomes and overall health and reduce health care costs. Provider status would align reimbursement with the services pharmacists are trained to provide and give underserved patients more access to crucial care.
What is the Pharmacy and Medically Underserved Areas Enhancement Act?
We call on Congress to improve patients’ access to health care by passing the Pharmacy and Medically Underserved Areas Enhancement Act, H.R. 2759/S. 1362. The bill would add pharmacists to the list of providers whose patient care services, when delivered to patients in medically underserved communities, are covered by Medicare Part B (i.e., grant them “provider status”). The legislation would ensure that pharmacists are fairly compensated for the valuable patient care they provide to beneficiaries who struggle to access basic health care services.
What is the top priority for pharmacy?
Pharmacy’s Top Priority: Medicare Provider Status Recognition. The profession’s flagship legislation, the Pharmacy and Medically Underserved Areas Enhancement Act, H.R. 2759/S. 1362 , was introduced in the U.S. House of Representatives on April 22, 2021 and the U.S. Senate on April 26, 2021.
Can a pharmacist bill Medicare?
Pharmacists offer services well beyond dispensing medications, and each state has its own scope of practice law that outlines which services they are authorized to provide. If Congress passed the Pharmacy and Medically Underserved Areas Enhancement Act, H.R. 2759/S. 1362 , pharmacists could bill Medicare Part B for services within their states’ scope of practice. Although they vary from state to state, these services generally include medication management, point-of-care testing, immunizations, and chronic disease management.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly. If you’re worried about paying for them after your Medicare coverage ends, talk to your doctor, nurse, or social worker.
How long does Medicare cover after kidney transplant?
If you're entitled to Medicare only because of ESRD, your Medicare coverage ends 36 months after the month of the kidney transplant. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly.
What is a prodrug?
A prodrug is an oral form of a drug that, when ingested, breaks down into the same active ingredient found in the injectable drug. As new oral cancer drugs become available, Part B may cover them. If Part B doesn’t cover them, Part D does.
What happens if you get a drug that Part B doesn't cover?
If you get drugs that Part B doesn’t cover in a hospital outpatient setting, you pay 100% for the drugs, unless you have Medicare drug coverage (Part D) or other drug coverage. In that case, what you pay depends on whether your drug plan covers the drug, and whether the hospital is in your plan’s network. Contact your plan to find out ...
What is Part B covered by Medicare?
Here are some examples of drugs Part B covers: Drugs used with an item of durable medical equipment (DME) : Medicare covers drugs infused through DME, like an infusion pump or a nebulizer, if the drug used with the pump is reasonable and necessary.
Does Medicare cover transplant drugs?
Medicare covers transplant drug therapy if Medicare helped pay for your organ transplant. Part D covers transplant drugs that Part B doesn't cover. If you have ESRD and Original Medicare, you may join a Medicare drug plan.
What is a pharmacist?
Pharmacists are trained and qualified to administer immunizations, measure and monitor blood pressure and cholesterol, perform foot checks for patients with diabetes, furnish smoking cessation products, screen for depression and other mental health conditions, and more.
What is the Pharmacy and Medically Underserved Areas Enhancement Act?
1362, seeks to improve health outcomes and lower health care spending by giving Medicare beneficiaries living in medically underserved communities access to patient care services from their state-licensed pharmacist.
What are the services of a pharmacist?
Pharmacists’ patient care services 1 Pharmacists are trained and qualified to administer immunizations, measure and monitor blood pressure and cholesterol, perform foot checks for patients with diabetes, furnish smoking cessation products, screen for depression and other mental health conditions, and more. Pharmacists can also perform point-of-care testing for blood glucose, cholesterol, influenza, strep, COVID-19, and more. 2 Pharmacists can educate and counsel patients to help them stay healthy while reducing cost burdens on payers. Counseling and education may include how to:#N#Find the best medication, use medications and devices (e.g., inhalers, nebulizers) correctly, manage medications that are ineffective, and identify more affordable medication options.#N#More safely use opioids or switch to nonopioid treatments for chronic pain.#N#Manage chronic disease. 3 Pharmacists are an important part of the comprehensive health care team. They work closely with their patients’ other health care providers to enhance quality of care, improve health outcomes, and save money for the patient and health care system.
Why is it important to have a pharmacist?
Pharmacists are an important part of the comprehensive health care team. They work closely with their patients’ other health care providers to enhance quality of care, improve health outcomes, and save money for the patient and health care system.
What is the National Association of Chain Drug Stores?
At present, the National Association of Chain Drug Stores, the American Public Health Association, the National Community Pharmacists Association , and numerous other organizations are all working toward this common goal: to encourage realization of the viability of pharmacists as qualified providers.
When is pharmacist month 2020?
October 7, 2020. Debbie Weitzman, President of Pharmaceutical Distribution, Cardinal Health. During American Pharmacists Month, and as the country uses all available health care resources to address COVID-19, there has never been a better or more important time to grant provider status to pharmacists. Throughout the coronavirus disease 2019 ...
Can pharmacists be part of Medicare?
Although pharmacists are valued community health care providers and their ability to improve outcomes as part of a patient’s care team has been proven, as of October 2020, only 37 states allowed pharmacists to qualify as medical providers under the rules of Medicare Part B. Because of this, pharmacists face administrative barriers when seeking reimbursement for clinical services provided.
Did pharmacists get ostracized from the HEALS Act?
Nonetheless, pharmacists were ostracized from the HEALS Act, the Senate’s $1 trillion coronavirus stimulus legislative package, excluding them from the expansion of testing and immunization.
Can pharmacies get reimbursement for emergency services?
In its 2017 report on public health and community partnerships, the Johns Hopkins Center for Health Security noted that some pharmacies historically have been unable to obtain reimbursement from payers for emergency services provided outside of their normal authorized scope of practice.
Can a pharmacist be a Medicare Part B provider?
Before a pharmacist can legally provide services, their state must first authorize these services under its legal SOP. If they are granted Medicare Part B provider status, more pharmacists would be authorized to provide patients with an expanded set of services, reducing the current burden on other sites of care.
Why is it important for pharmacists to bill for patient care services under Medicare Part B?
Use these Quick Facts to explain how authorizing pharmacists to bill for patient care services under Medicare Part B improves access to health care and improves outcomes in underserved communities.
Why are pharmacists considered providers?
Evidence shows that pharmacists make a significant impact on patients’ health outcomes and overall health and reduce health care costs. Provider status would align reimbursement with the services pharmacists are trained to provide and give underserved patients more access to crucial care.
What is the Pharmacy and Medically Underserved Areas Enhancement Act?
We call on Congress to improve patients’ access to health care by passing the Pharmacy and Medically Underserved Areas Enhancement Act, H.R. 2759/S. 1362. The bill would add pharmacists to the list of providers whose patient care services, when delivered to patients in medically underserved communities, are covered by Medicare Part B (i.e., grant them “provider status”). The legislation would ensure that pharmacists are fairly compensated for the valuable patient care they provide to beneficiaries who struggle to access basic health care services.
What is the top priority for pharmacy?
Pharmacy’s Top Priority: Medicare Provider Status Recognition. The profession’s flagship legislation, the Pharmacy and Medically Underserved Areas Enhancement Act, H.R. 2759/S. 1362 , was introduced in the U.S. House of Representatives on April 22, 2021 and the U.S. Senate on April 26, 2021.
Can a pharmacist bill Medicare?
Pharmacists offer services well beyond dispensing medications, and each state has its own scope of practice law that outlines which services they are authorized to provide. If Congress passed the Pharmacy and Medically Underserved Areas Enhancement Act, H.R. 2759/S. 1362 , pharmacists could bill Medicare Part B for services within their states’ scope of practice. Although they vary from state to state, these services generally include medication management, point-of-care testing, immunizations, and chronic disease management.