How much will Medicare spending increase in 2020?
Total Medicare spending is projected to increase from $523 billion in 2010 to around $900 billion by 2020. From 2010 to 2030, Medicare enrollment is projected to increase dramatically, from 47 million to 79 million, and the ratio of workers to enrollees is expected to decrease from 3.7 to 2.4.
How many people have Medicare in 2021?
The Patient Protection and Affordable Care Act of 2010 includes a long list of reform provisions intended to contain Medicare costs while increasing revenue, improving and streamlining its delivery systems, and even increasing services to the program. As of August 2021, there were nearly 63.8 million people enrolled in Medicare.
When did Medicare take effect?
In 1966, Medicare’s coverage took effect, as Americans age 65 and older were enrolled in Part A and millions of other seniors signed up for Part B. Nineteen million individuals signed up for Medicare during its first year. In 1972, President Richard M. Nixon signed into the law the first major change to Medicare.
What is the Medicare for all act of 2019?
To establish a Medicare-for-all national health insurance program. Be it enacted by the Senate and House of Representatives of the United States of America in Congress assembled, SECTION 1. Short title; table of contents. (a) Short title .—This Act may be cited as the “Medicare for All Act of 2019”.
What is in the new bill for Medicare?
Specifically, the bill would extend the moratorium on the 2% Medicare sequester cuts until April 1, 2022, and reduce the cuts from 2% to 1% from April 1 through June 30, 2022. The package also would stop the 4% statutory Pay-As-You-Go sequester from taking effect early next year.
What legislation enacted Medicare?
On July 30, 1965, President Lyndon B. Johnson signed the Medicare and Medicaid Act, also known as the Social Security Amendments of 1965, into law. It established Medicare, a health insurance program for the elderly, and Medicaid, a health insurance program for people with limited income.
What did the Medicare Act change?
Nixon signed into the law the first major change to Medicare. The legislation expanded coverage to include individuals under the age of 65 with long-term disabilities and individuals with end-stage renal disease (ERSD).
When was Medicare amended?
July 30, 1965The Social Security Amendments of 1965, Pub. L. 89–97, 79 Stat. 286, enacted July 30, 1965, was legislation in the United States whose most important provisions resulted in creation of two programs: Medicare and Medicaid....Social Security Amendments of 1965.CitationsActs amendedSocial Security ActLegislative history9 more rows
What is the Medicare for All Act of 2021?
The Medicare for All Act builds upon and expands Medicare to provide comprehensive benefits to every person in the United States. This includes primary care, vision, dental, prescription drugs, mental health, substance abuse, long-term services and supports, reproductive health care, and more.
Why was the Medicare Act created?
On July 30, 1965, President Lyndon B. Johnson signed into law legislation that established the Medicare and Medicaid programs. For 50 years, these programs have been protecting the health and well-being of millions of American families, saving lives, and improving the economic security of our nation.
What changes may occur for Medicare benefits in the next 20 years?
8 big changes to Medicare in 2020Part B premiums increased. ... Part B deductible increased. ... Part A premiums. ... Part A deductibles. ... Part A coinsurance. ... Medigap Plans C and F are no longer available to newly eligible enrollees. ... Medicare Plan Finder gets an upgrade for the first time in a decade.More items...
How has Medicare changed over the years?
Medicare has expanded several times since it was first signed into law in 1965. Today Medicare offers prescription drug plans and private Medicare Advantage plans to suit your needs and budget. Medicare costs rose for the 2021 plan year, but some additional coverage was also added.
What are the purposes of Medicare regulations?
Medicare Regulations means that certain government-sponsored insurance program under Title XVIII, P.L. 89-97, of the Social Security Act, which, among other things, provides for a health insurance system for eligible elderly and disabled individuals, as set forth at Section 1395, et seq.
What legislation has been enacted to ensure the quality of healthcare for Medicare eligible beneficiaries?
Barack Obama signs the Affordable Care Act (ACA), which strengthens Medicare coverage of preventive care, reduces beneficiary liability for prescription drug costs, institutes reforms of many payment and delivery systems, and creates the Center for Medicare and Medicaid Innovation.
When did Medicare Part C start?
The Balanced Budget Act of 1997 (BBA) established a new Part C of the Medicare program, known then as the Medicare+Choice (M+C) program, effective January 1999.
When did Medicare supplement plans became standardized?
Medicare SELECT was authorized by OBRA-1990 as a 15-State demonstration and became a national program in 1995.
How many people will have Medicare in 2021?
As of 2021, 63.1 million Americans had coverage through Medicare. Medicare spending is expected to account for 18% of total federal spending by 2028. Medicare per-capita spending grew at a slower pace between 2010 and 2017. Discussion about a national health insurance system for Americans goes all the way back to the days ...
How much will Medicare be spent in 2028?
Medicare spending projections fluctuate with time, but as of 2018, Medicare spending was expected to account for 18 percent of total federal spending by 2028, up from 15 percent in 2017. And the Medicare Part A trust fund was expected to be depleted by 2026.
How many QMBs were there in 2016?
In 2016, there were 7.5 million Medicare beneficiaries who were QMBs, and Medicaid funding was being used to cover their Medicare premiums and cost-sharing. To be considered a QMB, you have to be eligible for Medicare and have income that doesn’t exceed 100 percent of the federal poverty level. The ’90s.
How much was Medicare in 1965?
In 1965, the budget for Medicare was around $10 billion. In 1966, Medicare’s coverage took effect, as Americans age 65 and older were enrolled in Part A and millions of other seniors signed up for Part B. Nineteen million individuals signed up for Medicare during its first year. The ’70s.
What is the Patient Protection and Affordable Care Act?
The Patient Protection and Affordable Care Act of 2010 includes a long list of reform provisions intended to contain Medicare costs while increasing revenue, improving and streamlining its delivery systems, and even increasing services to the program.
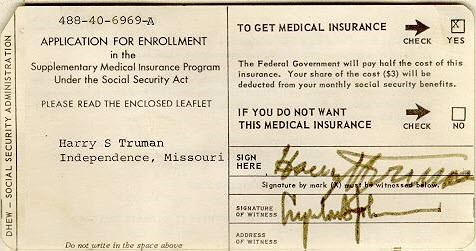
What was Truman's plan for Medicare?
The plan Truman envisioned would provide health coverage to individuals, paying for such typical expenses as doctor visits, hospital visits, ...
When did Medicare start?
But it wasn’t until after 1966 – after legislation was signed by President Lyndon B Johnson in 1965 – that Americans started receiving Medicare health coverage when Medicare’s hospital and medical insurance benefits first took effect. Harry Truman and his wife, Bess, were the first two Medicare beneficiaries.
What is the Medicare for All Act?
To establish a Medicare-for-all national health insurance program. Be it enacted by the Senate and House of Representatives of the United States of America in Congress assembled, SECTION 1. Short title; table of contents. (a) Short title .—This Act may be cited as the “Medicare for All Act of 2019”.
What is considered a qualified provider?
Qualifications for providers. (a) In general .—A health care provider is considered to be qualified to provide covered services if the provider is licensed or certified and meets—. (1) all the requirements of State law to provide such services; and. (2) applicable requirements of Federal law to provide such services.
How much does Medicare Part B cost in 2020?
Medicare D premiums are also higher for enrollees with higher incomes .
How many Medicare Advantage plans will be available in 2021?
For 2021, there are 21 Medicare Advantage and/or Part D plans with five stars. CMS noted that more than three-quarters of all Medicare beneficiaries enrolled in Medicare Advantage plans with integrated Part D prescription coverage would be in plans with at least four stars as of 2021.
What is Medicare D subsidy?
When Medicare D was created, it included a provision to provide a subsidy to employers who continued to offer prescription drug coverage to their retirees, as long as the drug covered was at least as good as Medicare D. The subsidy amounts to 28 percent of what the employer spends on retiree drug costs.
How did the ACA reduce Medicare costs?
Cost savings through Medicare Advantage. The ACA gradually reduced costs by restructuring payments to Medicare Advantage, based on the fact that the government was spending more money per enrollee for Medicare Advantage than for Original Medicare. But implementing the cuts has been a bit of an uphill battle.
Why did Medicare enrollment drop?
When the ACA was enacted, there were expectations that Medicare Advantage enrollment would drop because the payment cuts would trigger benefit reductions and premium increases that would drive enrollees away from Medicare Advantage plans.
What percentage of Medicare donut holes are paid?
The issue was addressed immediately by the ACA, which began phasing in coverage adjustments to ensure that enrollees will pay only 25 percent of “donut hole” expenses by 2020, compared to 100 percent in 2010 and before.
How many Medicare Advantage enrollees are there in 2019?
However, those concerns have turned out to be unfounded. In 2019, there were 22 million Medicare Advantage enrollees, and enrollment in Advantage plans had been steadily growing since 2004.; Medicare Advantage now accounts for well over a third of all Medicare beneficiaries.
How much is Medicare sequestration in FY2023?
In FY2023, the Medicare payment reductions are to be 2.90% for the first six months in which the sequestration order is effective and, for the second six months, the payment reduction is to be 1.11%. Hospitals.
When did Medicare extend outpatient therapy?
Revised requirements for Medicare payments for outpatient therapy services, including extending through December 31, 2013 the process allowing exceptions to limits (caps) on medically necessary outpatient therapy services. Made reductions to Medicare payments for multiple therapy services provided to the same patient on ...
What is Medicare Dependent Hospital Program?
Extended the Medicare Dependent Hospital Program (MDH) through FY2013 to allow qualifying small rural hospitals with a high proportion of Medicare patients to continue receiving Medicare payment adjustments. Extended the additional Medicare payment for inpatient services for low-volume hospitals through FY2013. Under the low-volume hospital extension, hospitals with fewer than 1,600 Medicare discharges and that are 15 miles or more from the nearest like hospital receive a graduated payment adjustment of up to 25%. Upon expiration, the adjustment will revert to original standards of fewer than 200 total discharges and more than 25 road miles.
How long did the Medicare and Medicaid extension extend?
Amended the Medicare, Medicaid, and SCHIP Extension Act of 2007 to extend for an additional 4 years : 1) certain rules for payments to LTCH hospitals-within-hospitals, and 2) the delay in the 25% patient threshold payment adjustment.
What is a PAC provider?
Required that post-acute care (PAC) providers (defined as long-term care hospitals (LTCHs), inpatient rehabilitation facilities (IRFs), skilled nursing facilities (SNFs), and home health agencies (HHAs)) report standardized patient assessment data, data on quality measures, and data on resource use and other measures, all of which meet specified requirements. Required the data to be standardized and interoperable to allow for exchange of longitudinal information among PAC and other providers to better enable them to coordinate care, improve Medicare beneficiary outcomes, and enhance discharge planning. Required PAC providers to report the standardized patient assessment data (at minimum for patient admissions and discharges) by October 1, 2018 for LTCHs, IRFs, and SNFs, and by January 1, 2019 for HHAs. Also required the Secretary by those same dates to ensure a match between the patient assessment data submission and claims data submitted for that patient.
Why was Medicare created?
It was intended to provide basic coverage through one health insurance system, with a defined set of benefits. Reforms to Medicare should honor and maintain its core values to ensure its continued success for future generations.
When did Medicare extend to disabled people?
In 1972 Medicare coverage was extended to people with significant disabilities. But Medicare’s success in providing access to health care for millions of people is in danger. Ironically, the threat comes from private insurance plans.
What is the Medicare platform?
Medicare Platform: Principles to Improve Medicare for All Beneficiaries Now and In the Future. Improve Consumer Protections and Quality Coverage. Cap out-of-pocket costs in traditional Medicare [1] Require Medigap plans to be available to everyone in traditional Medicare, regardless of pre-existing conditions and age.
How to ensure Medicare is comprehensive?
Ensure traditional Medicare is comprehensive, simple to navigate, and affordable. Add oral health, audiology, and vision coverage for all beneficiaries in traditional Medicare. Increase low-income protections and reduce cost-sharing. Add coverage for long-term care.
Why was the nursing home billed for $13,000?
She went from a hospital to a nursing home and was being billed for $13,000 because the nursing home was out of her MA plan’s network. She had been told by both the hospital and nursing home staff that original Medicare would cover her nursing home stay, even though she had an MA plan. This is not true.
When did Newt Gingrich say Medicare would be privatized?
In 1995 Newt Gingrich predicted that privatization efforts would lead Medicare to wither on the vine. He said it was unwise to get rid of Medicare right away, but envisioned a time when it would no longer exist because beneficiaries would move to private insurance plans.
Is Medicare a success?
When Medicare was created in 1965 over 50% of everyone 65 or older had no health insurance. Private insurance failed to meet their needs. Medicare, on the other hand, is a success. It increased the number of insured older adults to 95%. In 1972 Medicare coverage was extended to people with significant disabilities. But Medicare’s success in providing access to health care for millions of people is in danger. Ironically, the threat comes from private insurance plans. Funded by windfall subsidies from taxpayer dollars, privatization is jeopardizing the cost-effective, dependable Medicare program.
When did Medicare expand?
Over the years, Congress has made changes to Medicare: More people have become eligible. For example, in 1972 , Medicare was expanded to cover the disabled, people with end-stage renal disease (ESRD) requiring dialysis or kidney transplant, and people 65 or older that select Medicare coverage.
How long has Medicare and Medicaid been around?
Medicare & Medicaid: keeping us healthy for 50 years. On July 30, 1965, President Lyndon B. Johnson signed into law legislation that established the Medicare and Medicaid programs. For 50 years, these programs have been protecting the health and well-being of millions of American families, saving lives, and improving the economic security ...
What is Medicare Part D?
Medicare Part D Prescription Drug benefit. The Medicare Prescription Drug Improvement and Modernization Act of 2003 (MMA) made the biggest changes to the Medicare in the program in 38 years. Under the MMA, private health plans approved by Medicare became known as Medicare Advantage Plans.
What is the Affordable Care Act?
The 2010 Affordable Care Act (ACA) brought the Health Insurance Marketplace, a single place where consumers can apply for and enroll in private health insurance plans. It also made new ways for us to design and test how to pay for and deliver health care.
When was the Children's Health Insurance Program created?
The Children’s Health Insurance Program (CHIP) was created in 1997 to give health insurance and preventive care to nearly 11 million, or 1 in 7, uninsured American children. Many of these children came from uninsured working families that earned too much to be eligible for Medicaid.
Does Medicaid cover cash assistance?
At first, Medicaid gave medical insurance to people getting cash assistance. Today, a much larger group is covered: States can tailor their Medicaid programs to best serve the people in their state, so there’s a wide variation in the services offered.
What is the Medicare readmission penalty for 2020?
The 2020 Medicare Readmission Penalty Program. Each year, Medicare analyzes the readmission rate for every hospital in the United States and then imposes financial penalties on those hospitals determined to have excessively high readmission rates. And every year, most U.S. hospitals get penalized. This year is no exception – 83% ...
How does Medicare respond to the penalty based on a given hospital’s patient demographics?
Medicare responded by making 2 adjustments to the penalty based on a given hospital’s patient demographics: The severity of illness of the hospital’s patients (often called the case mix index) with the premise that the sicker a patient is, the more likely that patient is to be readmitted to the hospital. The rate of “dual eligible” patients, that ...
What is the Medicare quintile?
Medicare divided all U.S. hospitals into quintiles based on the percentage of dual eligible patients. Hospitals were only compared to other hospitals within the same quintile for the purposes of penalty calculation; therefore, a hospital with a high percentage of dual eligible patients was held to a different readmission rate expectation ...
Why are hospitals financially incentivized to discharge patients?
Since hospitals are paid by the DRG (in other words, by the diagnosis), hospitals are financially incentivized to discharge patients as quickly as possible in order to reduce their expenses. The Medicare hospital readmission reduction program was designed to offset that financial incentive by penalizing hospitals that discharge patients prematurely.
