To qualify, you must:
- Be eligible for or enrolled in Medicare Parts A and B;
- Have countable income at or below 100% of the Federal Poverty Guidelines (FPG) ($1,074 per month, $1,452 for couples);
- Have resources at or below the limit ($8,400 for individuals, $12,600 for couples); and.
Does Someone on Medicaid automatically qualify for Medicare?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
Does my income affect my monthly premiums for Medicare?
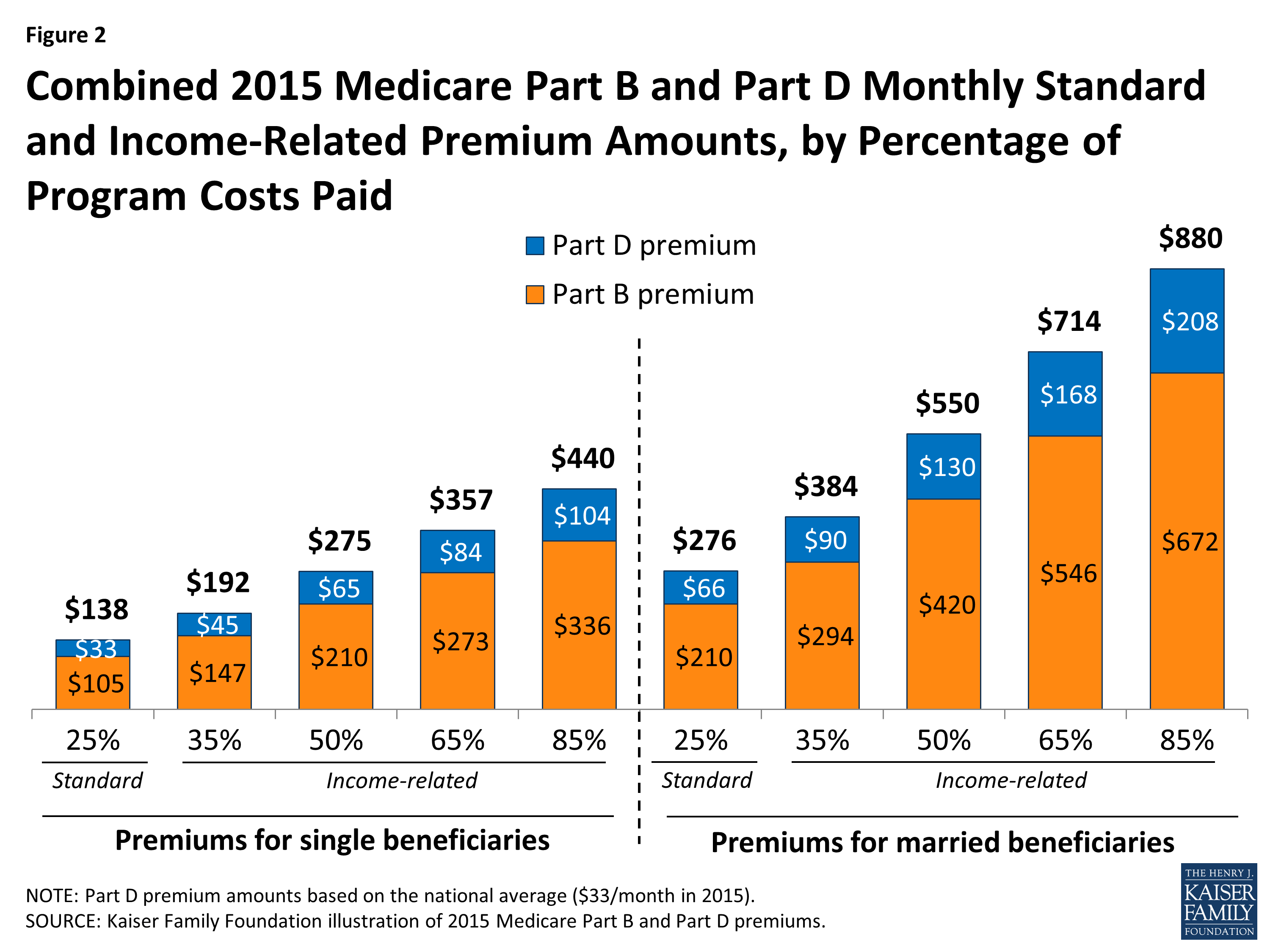
Most Medicare recipients will pay the standard premium. However, if Medicare sees that your tax return reported an income that exceeded the limit, your premiums will be adjusted to reflect that. This excess will be reflected as an Income Related Monthly Adjustment Amount (IRMAA), which is a surcharge added on to the standard premium.
What is the monthly income limit for Medicaid?
What are the income guidelines for Medicaid? Income requirements: For Medicaid coverage a single adult is capped $1,468 per month and families of four can make $3,013 per month. Single aged or disabled adults over 65 have an income cap of $836 and $1,195 for couples.
Are there limits to my Medicare coverage?
In general, there’s no upper dollar limit on Medicare benefits. As long as you’re using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.

What is the Medicare earnings limit for 2021?
In 2021, the adjustments will kick in for individuals with modified adjusted gross income above $88,000; for married couples who file a joint tax return, that amount is $176,000. For Part D prescription drug coverage, the additional amounts range from $12.30 to $77.10 with the same income thresholds applied.
What is the threshold of income for Medicare?
Qualified Medicare Beneficiary (QMB) program You can qualify for the QMB program if you have a monthly income of less than $1,094 and total resources of less than $7,970. For married couples, the limit is less than $1,472 monthly and less than $11,960 in total.
What income level triggers higher Medicare premiums?
If you file your taxes as “married, filing jointly” and your MAGI is greater than $170,000, you'll pay higher premiums for your Part B and Medicare prescription drug coverage. If you file your taxes using a different status, and your MAGI is greater than $85,000, you'll pay higher premiums.
Is Medicare based on your income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
Can you be denied Medicare?
In all but four states, insurance companies can deny private Medigap insurance policies to seniors after their initial enrollment in Medicare because of a pre-existing medical condition, such as diabetes or heart disease, except under limited, qualifying circumstances, a Kaiser Family Foundation analysis finds.
Do 401k withdrawals count as income for Medicare?
The distributions taken from a retirement account such as a traditional IRA, 401(k), 403(b) or 457 Plan are treated as taxable income if the contribution was made with pre-tax dollars, Mott said.
How much is the Medicare premium in 2020?
$144.60The Centers for Medicare & Medicaid Services has announced that the standard monthly Part B premium will be $144.60 in 2020, an increase from $135.50 in 2019. However, some Medicare beneficiaries will pay less than this amount.
How much does Social Security take out for Medicare each month?
The standard Medicare Part B premium for medical insurance in 2021 is $148.50. Some people who collect Social Security benefits and have their Part B premiums deducted from their payment will pay less.
What are Medicare income limits?
Medicare beneficiaries with incomes above a certain threshold are charged higher premiums for Medicare Part B and Part D. The premium surcharge is...
Why does Medicare impose income limits?
The higher premiums for Part B took effect in 2007, under the Medicare Modernization Act. And for Part D, they took effect in 2011, under the Affor...
Who is affected by the IRMAA surcharges and how does this change over time?
There have been a few recent changes that affect high-income Medicare beneficiaries: In 2019, a new income bracket was added at the high end of the...
Will there be a rate increase in 2022?
We don’t yet have concrete details from CMS. But the Medicare Trustees Report, which was published in late August, projects that the standard Part...
How much does Medicare pay for Part D?
If you earn more than $88,000 but less than $412,000, you’ll pay $70.70 on top of your plan premium. If you earn $412,000 or more, you’ll pay $77.10 in addition to your plan premium. Medicare will bill you for the additional Part D fee every month.
How much do you have to pay in taxes if you make more than $412,000 a year?
If you earn more than $412,000 per year, you’ll have to pay $504.90 per month in taxes. Part B premiums will be cut off directly from your Social Security or Railroad Retirement Board benefits. Medicare will send you a fee every three months if you do not receive either benefit.
What is SLMB in Medicare?
SLMB, or Specified Low-Income Medicare Beneficiary. If you earn less than $1,296 per month and have less than $7,860 in assets, you may be eligible for SLMB. Married couples must make less than $1,744 per month and have less than $11,800 in debt to qualify. This plan covers your Part B premiums.
What happens if you retire in 2020 and only make $65,000?
Loss of income from another source. If you were employed in 2019 and earned $120,000 but retired in 2020 and now only make $65,000 from benefits, you may want to challenge your IRMAA. To keep track of your income fluctuations, fill out the Medicare Income-Related Monthly Adjustment Amount – Life-Changing Event form.
What is the income limit for QDWI?
You must meet the following income criteria if you want to enroll in your state’s QDWI program: Individuals must have a monthly income of $4,339 or less and a $4,000 resource limit. A married couple’s monthly income must be less than $5,833. A married couple’s resource limit must be less than $6,000.
How much do you have to pay for Part B?
If this is the case, you must pay the following amounts for Part B: If you earn less than $88,000 per year, you must pay $148.50 per month. If you earn more than $88,000 but less than $412,000 per year, you must pay $475.20 per month.
Is there a higher income limit for Medicaid in Hawaii?
The income limits are higher in Alaska and Hawaii for all programs. Furthermore, even if your income is slightly above the cap, you may be eligible for these programs if it comes from a job and benefits. If you believe you may qualify for Medicaid, contact the Medicaid office in your state.
4 kinds of Medicare Savings Programs
Select a program name below for details about each Medicare Savings Program. If you have income from working, you still may qualify for these 4 programs even if your income is higher than the income limits listed for each program.
How do I apply for Medicare Savings Programs?
If you answer yes to these 3 questions, call your State Medicaid Program to see if you qualify for a Medicare Savings Program in your state:.
What is the income limit for extra help in 2021?
What Are the Income and Resource Limits for Extra Help in 2021? In 2021, the annual income limit for Extra Help for an individual is $19,140. For a married couple who is living together, the limit is $25,860. When your income is calculated, governmental assistance such as food stamps, housing assistance, and home energy assistance aren’t counted.
How much does a generic prescription cost?
For those enrolled in Extra Help, generic prescription costs are no more than $3.60 each, and brand-name prescription costs are no more than $8.95 each. If you didn’t enroll in Part D when you first became eligible, you won’t have to pay the late enrollment penalty if you have Extra Help.
How much does extra help save?
On average, Extra Help is estimated to save beneficiaries $5,000 in these costs per year. If you’re eligible for Medicaid or any of the following Medicare Savings Programs, you automatically qualify for Extra Help. Qualified Medicare Beneficiary (QMB)
Can you mail a color coded document to Medicare?
You can mail your color-coded document to your Part D plan to help verify the level of Extra Help for which you qualify. Those who are dual-eligible to receive Medicare and Medicaid qualify for full Extra Help.
Is food stamps counted as extra help?
When your income is calculated, governmental assistance such as food stamps, housing assistance, and home energy assistance aren’t counted. Even if your income is higher than the limits, you should still apply for Extra Help if you think you qualify. Some scenarios where you’d still be eligible for Extra Help even though your income is over ...
What is QI in Medicare?
Qualifying Individual (QI) Programs are also known as additional Low-Income Medicare Beneficiary (ALMB) programs. They offer the same benefit of paying the Part B premium, as does the SLMB program, but you can qualify with a higher income. Those who qualify are also automatically eligible for Extra Help.
What is Medicare Savings Program?
A Medicare Savings Program (MSP) can help pay deductibles, coinsurance, and other expenses that aren’t ordinarily covered by Medicare. We’re here to help you understand the different types of MSPs. Below, we explain who is eligible for these programs and how to get the assistance you need to pay for your Medicare.
Does Medicare savers have a penalty?
Also, those that qualify for a Medicare Savings Program may not be subject to a Part D or Part B penalty. Although, this depends on your level of extra help and the state you reside in. Call the number above today to get rate quotes for your area.
For those who qualify, there are multiple ways to have your Medicare Part B premium paid
In 2022, the standard Medicare Part B monthly premium is $170.10. Beneficiaries also have a $233 deductible, and once they meet the deductible, must typically pay 20% of the Medicare-approved amount for any medical services and supplies.
What is the Part B premium reduction benefit?
The giveback benefit, or Part B premium reduction, is when a Part C Medicare Advantage (MA) plan reduces the amount you pay toward your Part B monthly premium. Your reimbursement amount could range from less than $1 to the full premium amount, which is $170.10 in 2022.
How to find plans that offer the giveback benefit
Not all MA plans offer this benefit, so you must find a plan that does in order to take advantage of the opportunity. In 2022, these plans are offered in nearly all states, so you may find one close to you.
Other Part B reimbursement options
There are other ways you can lower or eliminate how much you pay for the Medicare Part B premium. This includes certain Medicaid programs or benefits from some retiree health plans.
What are the expenses that go away when you receive Medicaid at home?
When persons receive Medicaid services at home or “in the community” meaning not in a nursing home through a Medicaid waiver, they still have expenses that must be paid. Rent, mortgages, food and utilities are all expenses that go away when one is in a nursing home but persist when one receives Medicaid at home.
How long does it take to get a medicaid test?
A free, non-binding Medicaid eligibility test is available here. This test takes approximately 3 minutes to complete. Readers should be aware the maximum income limits change dependent on the marital status of the applicant, whether a spouse is also applying for Medicaid and the type of Medicaid for which they are applying.
Is income the only eligibility factor for Medicaid?
Medicaid Eligibility Income Chart by State – Updated Mar. 2021. The table below shows Medicaid’s monthly income limits by state for seniors. However, income is not the only eligibility factor for Medicaid long term care, there are asset limits and level of care requirements.
