The Medicare claims appeal process has five levels:
- Redetermination. The first step in the Medicare appeals process is a review of the initial determination made by the company that handles Medicare claims. ...
- Reconsideration. ...
- Administrative law judge (ALJ) hearing. ...
- Medicare Appeals Council review. ...
- Judicial review in U.S. ...
Full Answer
How does the Medicare appeals process work?
What’s the appeals process for Original Medicare? The appeals process has 5 levels: Level 1: Redetermination by the Medicare Administrative Contractor (MAC) Level 2: Reconsideration by a Qualified Independent Contractor (QIC) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council (Appeals Council)
What are the levels of Medicare Appeals?
Medicare FFS has 5 appeal process levels: Level 1 - MAC Redetermination Level 2 - Qualified Independent Contractor (QIC) Reconsideration Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition Level 4 - Medicare Appeals Council (Council) Review Level 5 - U.S. District Court Judicial Review Make all appeal requests in writing.
How to properly compose Medicare appeal letter and its sample?
OMHA is responsible for Level 3 claims appeals. The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan. There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you …
What is second level Medicare appeal?
Aug 31, 2019 · If you did not succeed in a Level 2 appeal, you can complete a Request for Medicare Hearing by an Administrative Law Judge (ALJ) Form or send a written request to the specific Office of Medicare Hearings and Appeals (OMHA) Central Operations listed on your Level 2 denial letter. In theory, you will get a Level 3 hearing within 90 days, but there is an …

What are the five steps in the Medicare appeals process?
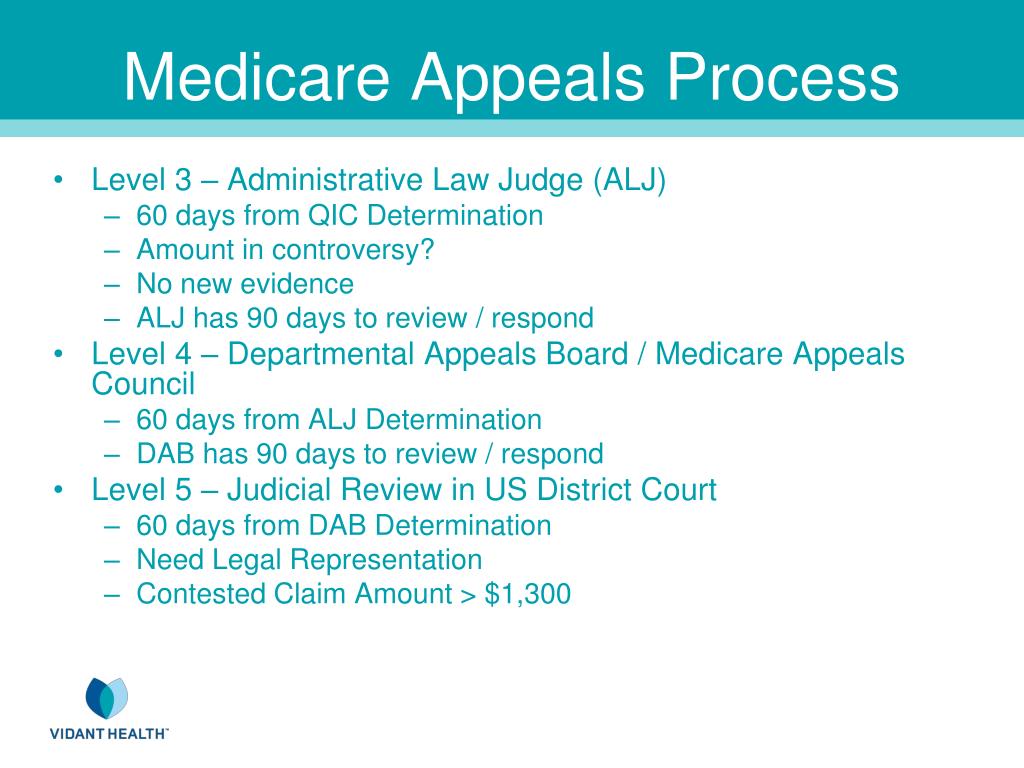
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
How many steps are there in the Medicare appeal process?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
What is the first step in the Medicare appeals process?
The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim.
What are the chances of winning a Medicare appeal?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
Which of the following is the highest level of the appeals process of Medicare?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
What is the highest level of a Medicare Redetermination?
Medicare FFS has 5 appeal process levels:Level 1 - MAC Redetermination.Level 2 - Qualified Independent Contractor (QIC) Reconsideration.Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition.Level 4 - Medicare Appeals Council (Council) Review.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
Who pays if Medicare denies a claim?
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure.
Can Medicare deny treatment?
Absolutely. Sometimes Medicare will decide that a particular treatment or service is not covered and will deny a beneficiary's claim.
Who has right to appeal?
To stress, the right to appeal is statutory and one who seeks to avail of it must comply with the statute or rules. The requirements for perfecting an appeal within the reglementary period specified in the law must be strictly followed as they are considered indispensable interdictions against needless delays.Apr 10, 2013
How do I get a Medicare denial letter?
When Medicare refuses to pay for a prescribed drug, an individual can request a coverage determination or an exception by completing a “Model Coverage Determination Request” form or writing a letter of explanation.Aug 20, 2020
What is a 2nd level appeal?
Second Level of Appeal: Reconsideration by a Qualified Independent Contractor. Any party to the redetermination that is dissatisfied with the decision may request a reconsideration.Apr 4, 2022
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
What is a QIC?
QIC is an independent contractor that didn’t take part in the level 1 decision. The QIC will review your request for a reconsideration and will make a decision.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Can you request a fast reconsideration?
If you disagree with the plan’s redetermination, you, your representative, or your doctor or other prescriber can request a standard or expedited (fast) reconsideration by an IRE. You can’t request a fast reconsideration if it’s an appeal about payment for a drug you already got.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What does "I" mean in CMS?
In a 2019 Final Rule, CMS ended the requirement that appellants sign their appeal requests.In this booklet, “I” or “you” refers to patients, parties, and appellants active in an appeal.
Can a patient transfer their appeal rights?
Patients may transfer their appeal rights to non-participating providers or suppliers who provide the items or services and don’t otherwise have appeal rights. To transfer appeal rights, the patient and non-participating provider or supplier must complete and sign the
What happens if you disagree with an ALJ?
If you disagree with the ALJ or attorney adjudicator decision, or you wish to escalate your appeal because the OMHA adjudication time frame passed, you may request a Council review. The Council is part of the HHS Departmental Appeals Board (DAB).
What are the levels of Medicare appeal?
There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim. Level 2: An Independent Organization . If you disagree with the decision in Level 1 , you may request a reconsideration by an independent organization.
What is the OMHA level 3?
OMHA is responsible for Level 3 claims appeals. The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan.
How to appeal a Medicare claim?
Medicare allows you to pursue an appeal in one of three ways: 1 Follow the appeals instructions included with your MSN and send a copy of the MSN and all requested documents to the company that processed your claim. 2 Complete the Centers for Medicare and Medicaid Services Redetermination Request Form and send it to the company that processed your claim. 3 Write a letter directly to the company that processed your claim that includes your name, Medicare number, denied service, and the reason why you are requesting an appeal.
What is Medicare summary notice?
The Medicare Summary Notice (MSN) is a form you will receive quarterly (every three months) that lists all the Medicare services you received during that time, the amount that Medicare paid, and any non-covered charges, among other information. 1 Please note that the MSN is sent to people on Original Medicare ( Part A and Part B ), not to people on Medicare Advantage. It is not a bill and may be sent to you from the company assigned to process your Medicare claim, not from Medicare itself.
How many levels of appeals are there for Medicare?
There are five levels in the Medicare appeals process. 2 If at any time your appeal is approved by Medicare, the process ends at the level you are currently on. If a denial is upheld, you will have to decide whether or not to proceed to the next level.
Does Medicare cover everything?
on April 03, 2020. Medicare does not cover everything, even when you think it will. Odds are you will face a coverage denial at some point in time. Understanding how the Medical appeals process works will not only save you time and frustration, it will also improve your chances of getting those services covered.
How long does it take to get a level 1 decision?
You will get a Level 1 decision within 60 days. It could take an additional 14 days, however, if you submit additional information after the case was filed. If your claim is denied at Level 1, you have 180 days to proceed to the next level.
Who is Lisa Sullivan?
Fact checked by Lisa Sullivan, MS on April 03, 2020. Lisa Sullivan, MS, is a nutritionist and a corporate health and wellness educator with nearly 20 years of experience in the healthcare industry. Learn about our editorial process. Lisa Sullivan, MS. on April 03, 2020.
What is the Medicare Appeals Council?
The Medicare Appeals Council (Council) reviews appeals of ALJ decisions. The Council’s Administrative Appeals Judges are located within the HHS Departmental Appeals Board (DAB), and the Council is independent of both CMS and OMHA. The Council provides the final administrative review for Medicare claim appeals. Parties dissatisfied with the outcome of an ALJ decision have 60 days from the date of receipt of the ALJ’s decision to file a request for Council review. Appellants may also file a request with the Council to escalate an appeal from the ALJ level if the ALJ has not completed his or her action on the request for hearing within the adjudication deadline. Section 1869(d)(2)(A) of the Act contemplates that the Council render a decision or remand the case to the ALJ within 90 days from the date the request for review is timely filed. If the Council does not render a decision within 90 days, the appellant may request that the appeal be escalated to Federal district court. Due to an overwhelming number of Council review requests over the past several years, the Council has not been able to meet the 90-day timeframe for adjudication in some cases, resulting in a backlog of appeals at the Council.
How long does it take to get a redetermination from a MAC?
The Act does not require a minimum amount-in-controversy. The Act contemplates that the MAC is to complete a redetermination within 60 days after the MAC receives the request for redetermination.
When did Medicare start increasing?
Beginning in 2011, Medicare began experiencing a large increase in the number of new beneficiaries as members of the “baby boom” generation reached 65 and became eligible for Medicare. This, coupled with recent increases in the number of younger disabled individuals enrolling in Medicare, and beneficiaries living longer, has caused increases in the Medicare services provided. This increase in the number of Medicare claims has had a commensurate impact on the number of potential denials of payment and has led to increased appeals of disputed claims. While these increases in the number of appeals were expected, funding to adjudicate them has remained comparatively stagnant.
How long does it take to get a QIC reconsideration?
If a party is dissatisfied with a QIC reconsideration, the party has 60 days from the date of receipt of the QIC reconsideration to file a request for a hearing before an ALJ at the Office of Medicare Hearings and Appeals (OMHA), which is independent from CMS. This provides parties a fair and impartial forum to address disagreements with CMS Medicare coverage and payment determinations. A minimum amountin-controversy is required for a hearing (the amount is adjusted annually based on a formula prescribed by statute; and for 2017, the minimum amount-in-controversy for a claim appealed to OMHA is $160). Section 1869(d)(1)(A) of the Act contemplates that an ALJ conduct a hearing and render a decision within 90 days beginning on the date the request for hearing is filed. If the ALJ does not render a decision within the timeframe contemplated by the Act, the party that requested the hearing may request a review by the Medicare Appeals Council at the HHS Departmental Appeals Board (DAB). Due to an overwhelming number of hearing requests over the past several years, OMHA has not been able to meet the 90-day time-frame for adjudication in some cases, resulting in a backlog of appeals at OMHA.
What is Medicare appeal?
It helps to provide evidence that supports your appeals case from a doctor or other provider. There might be times when Medicare denies your coverage for an item, service, or test. You have the right to formally disagree with this decision and encourage Medicare to change it. This process is called a Medicare appeal.
How many levels of appeals are there?
The appeals process has five levels. Each level is a different review process with a different timetable. You’ll need to request an appeal at each level. If your appeal is successful at the first level, or if you agree with Medicare’s reasoning for denying your appeal, you can stop there. However, if your appeal was denied ...
Can you appeal Medicare Part D?
You can use an appeal in a few different situations, such as denial of coverage for a test or service or if you’re charged a late fee you think is in error. No matter the situation, you’ll need to prove your case to Medicare.
What is a fast appeal?
In a few cases, you’ll file what’s called a fast appeal. Fast appeals apply when you’re notified that Medicare will no longer cover care that’s: at a hospital. at a skilled nursing facility. at a rehabilitation facility. in hospice.
How long does it take to get a decision from Medicare?
You’ll hear a decision about your appeal within 60 days.
Does Medicare cover prescriptions?
Medicare never covers the item, service, or prescription. You won’t be able to get coverage, even with an appeal, if it’s something Medicare never covers. However, if you think your item, service, or test is medically necessary or that you do meet the requirements, you can appeal.
What is an ABN in nursing?
An ABN lets you know that an item, service, or prescription won’t be covered or will no longer be covered. Skilled Nursing Facility Advance Beneficiary Notice (SNF ABN). An SNF ABN lets you know that Medicare will no longer be covering your stay in a skilled nursing facility.
medicare appeals process
Not every Medicare claim that is filed will process smoothly the first time around. However, it’s pretty common and obvious to the medical billing staff what went wrong. When this happens, fixing the problem and re-opening or resubmitting your claim can end up fixing the problem without the appeals process.
When can I appeal a claim?
You will be able to appeal a claim if Medicare or your health plan denies one of these 3:
How do I file my appeal?
There are multiple appeals processes. The appeals process is determined by where you are filing. It will be a different process depending on which of the following 3 situations you’re experiencing:
Appeals with Original Medicare
If you only have Original Medicare, then the first thing you need to do is find your “ Medicare Summary Notice ” (MSN). You need to file your appeal within 120 days of the date you received your Medicare Summary Notice.
Appeals with a Medicare health plan
When you have a Medicare health plan, like Medigap, then you should start the appeal process through your Medicare health plan.
Appeals with a Prescription Drug plan
If you have Medicare drug plan coverage, you will need to begin the appeal process through your PDP plan.