Explore
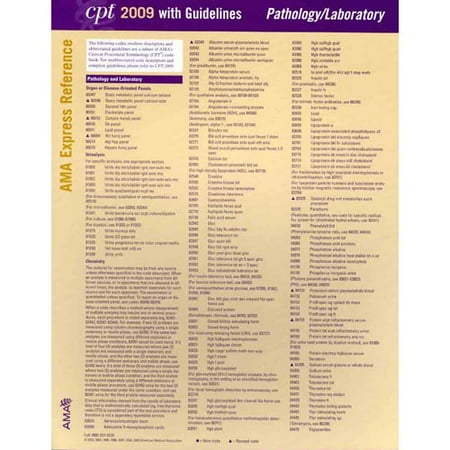
The Current Procedural Terminology (CPT) code range for Pathology and Laboratory Procedures 0001U-89398 is a medical code set maintained by the American Medical Association. Subscribe to Codify and get the code details in a flash.
What is the CPT code for lab testing?
There are 2 configurations for, Panel CPT code 80048: 1. A submission that includes 5 or more of the following laboratory Component Codes by the Same Individual Physician or Other Qualified Health Care Professional for the same patient on the same date of service is a reimbursable service as, Panel CPT code 80048. Panel Code: 80048
What is included in CPT code 80048?
codes - 86704 to 86706 TB Skin Test - 86580 . Title: Microsoft Word - CPT Codes for Titers Author: zahodnicr Created Date: 2/21/2012 7:32:54 AM ...
What is the CPT code for titer?
Laboratory Tests for which Medicare Allows One Test Without a Practitioner Order During the PHE* Updated May 5, 2021 . CPT/ HCPCS Code Laboratory Code Long Descriptor Target 1. COVID -19 Related Codes U0001 CDC 2019-nCoV Real-Time RT-PCR Diagnostic Panel COVID-19 U0002 2019-nCoV Coronavirus, SARS-CoV-2/2019-nCoV (COVID-19), any technique ...
What are lab test codes?
What is a PTT?
What is PTT in coagulation?
What is the purpose of PTT?
Is a thrombolytic test necessary?
Is PTT necessary for warfarin?
See more
About this website
What is the CPT code for PTT?
020321: Prothrombin Time (PT) and Partial Thromboplastin Time (PTT) | Labcorp.
What ICD 10 code covers PT PTT Medicare?
NCD - Partial ThromboplastinTime (PTT) (190.16)
What diagnosis codes cover PTT?
The PTT NCD includes in the covered list of ICD-9-CM diagnostic codes code V72. 81 (Pre-operative cardiovascular examination,) code V72. 83 (Other specified pre-operative examination,) and code V72. 84 (Pre-operative examination, unspecified).
What ICD 10 will cover PTT?
1.
Does Medicare cover prothrombin time test?
The Centers for Medicare & Medicaid Services (CMS) today expanded Medicare coverage for home blood testing of prothrombin time (PT) International Normalized Ratio (INR) to include beneficiaries who are using the drug warfarin, an anticoagulant (blood thinner) medication, for chronic atrial fibrillation or venous ...
What is the ICD-10 code for elevated PTT?
R79. 1 - Abnormal coagulation profile | ICD-10-CM.
Is 85610 covered by Medicare?
A: When physicians use a prothrombin time test (reported with CPT code 85610) to monitor patients on anticoagulant drugs, Medicare pays the entity that performed the test. Its payment for the test is based on the geographically specific laboratory test fee schedule.
What is the CPT code for PT INR?
Patient has an INR test at a lab in the office or at the point of care and follows up with a visit to discuss results. Report CPT codes 85610 (prothrombin time) and 93793. Patient presents for an office visit during which the physician also discusses INR monitoring.
Are aPTT and PTT the same?
The partial thromboplastin time (PTT; also known as activated partial thromboplastin time (aPTT)) is a screening test that helps evaluate a person's ability to appropriately form blood clots. It measures the number of seconds it takes for a clot to form in a sample of blood after substances (reagents) are added.
Does Medicare cover CPT code 83036?
(2) the service must be medically necessary or indicated. Once these two criteria are met, Medicare pays for most clinical laboratory tests based on the Laboratory Fee Schedule.
What is CPT code 85730 used for?
CPT® Code 85730 - Hematology and Coagulation Procedures - Codify by AAPC.
What is a PT and PTT blood test?
Definition. Partial thromboplastin time (PTT) is a blood test that looks at how long it takes for blood to clot. It can help tell if you have a bleeding problem or if your blood does not clot properly. A related blood test is prothrombin time (PT) .
Partial Thromboplastin Time (PTT) - Quest Diagnostics
CPT: Code Description Medicare National Coverage Determination Policy The ICD10 codes listed below are the top diagnosis codes currently utilized by ordering physicians
NCD - Blood Counts (190.15) - CMS
Item/Service Description. Blood counts are used to evaluate and diagnose diseases relating to abnormalities of the blood or bone marrow. These include primary disorders such as anemia, leukemia, polycythemia, thrombocytosis and thrombocytopenia.
Reimbursement Quick Reference Guide for Prothrombin Time/INR Testing
PN 100299 Rev AA CoaguSense, Inc. Effective Date: 4/9/2010 Page: 1 of 2 DCO: 733 Reimbursement Quick Reference Guide for Prothrombin Time/INR Testing
NCD - Prothrombin Time (PT) (190.17) - CMS
Item/Service Description. Basic plasma coagulation function is readily assessed with a few simple laboratory tests: the partial thromboplastin time (PTT), PT, thrombin time (TT), or a quantitative fibrinogen determination.
Prothrombin Time (PT) - Quest Diagnostics
CPT: Code Description Medicare National Coverage Determination Policy The ICD10 codes listed below are the top diagnosis codes currently utilized by ordering physicians
covered DX for CPT 83036 – 211.7,250.00 V58.69
Most used ICD 10 code GLYCOSYLATED HEMOGLOBIN (CPT 83036, 83037) ICD-10 Description ICD-10 ICD-9 Abnormal Finding Of Blood Chemistry, Unspecified R79.9 790.6
How to collect blood for coagulation?
1 Evacuated collection tubes must be filled to completion to ensure a proper blood to anticoagulant ratio. 2,3 The sample should be mixed immediately by gentle inversion at least six times to ensure adequate mixing of the anticoagulant with the blood. A discard tube is not required prior to collection of coagulation samples. 4,5 When noncitrate tubes are collected for other tests, collect sterile and nonadditive (red-top) tubes prior to citrate (blue-top) tubes. Any tube containing an alternate anticoagulant should be collected after the blue-top tube. Gel-barrier tubes and serum tubes with clot initiators should also be collected after the citrate tubes. To avoid delays in turnaround time when requesting multiple tests on frozen samples, please submit separate frozen specimens for each test requested.
Do you need a discard tube for coagulation?
A discard tube is not required prior to collection of coagulation samples. 4,5 When noncitrate tubes are collected for other tests, collect sterile and nonadditive (red-top) tubes prior to citrate (blue-top) tubes. Any tube containing an alternate anticoagulant should be collected after the blue-top tube. Gel-barrier tubes and serum tubes ...
What is the PT test for coagulation?
The PT test is one in-vitro laboratory test used to assess coagulation . While the PTT assesses the intrinsic limb of the coagulation system, the PT assesses the extrinsic or tissue factor dependent pathway. Both tests also evaluate the common coagulation pathway involving all the reactions that occur after the activation of factor X.
What is a PT in a thrombolytic?
A PT may be used to assess the risk of hemorrhage or thrombosis in patients who are going to have a medical intervention known to be associated with increased risk of bleeding or thrombosis . For example: evaluation prior to invasive procedures or operations of patients with personal history of bleeding or a condition associated with coagulopathy prior to the use of thrombolytic medication.
What is a PT for heparin?
A PT may be used to assess patients taking warfarin. The prothrombin time is generally not useful in monitoring patients receiving heparin who are not taking warfarin.
Is PT testing a self monitoring test?
Current medical information does not clarify the role of laboratory PT testing in patients who are self monitoring. Therefore, the indications for testing apply regardless of whether or not the patient is also PT self-testing.
Is INR a part of PT?
Since the INR is a calculation, it will not be paid in addition to the PT when expressed in seconds, and is considered part of the conventional PT test.
What is the aPTT reagent?
The aPTT reagent consisting of silica mixed with synthetic phospholipid is mixed with the patient plasma. The silica provides a negatively-charged particulate surface for the activation of the contact pathway of coagulation. Calcium chloride is then added to the sample/reagent mixture to initiate clot formation. The time to clot formation is measured photo-optically.
Why is aPTT ordered?
The aPTT is often ordered, along with the prothrombin time, to diagnose the cause of patient bleeding or as part of a presurgical screen to rule out coagulation defects. 9-11 The aPTT can be prolonged when the activities of any of the factors of the intrinsic pathway are significantly diminished.
What is the APTT LA?
The aPTT-LA is a more sensitive screening test for identifying lupus anticoagulants in patients with a history of thrombosis. The aPTT may not be extended in individual factor deficiencies unless the levels drop below 15% to 45% depending on the factor. 6 Less significant individual factor deficiencies in combination (multiple factor deficiency) can extend the aPTT. 6 The aPTT is more sensitive to intrinsic pathway factor deficiencies than common pathway factor deficiencies. 6 Factor VIII elevations, as can occur due to acute phase reactions, can normalize a mildly extended aPTT result. 6
What causes an extended aPTT?
An extended aPTT can be seen in acquired deficiencies of factors II, IX, and X that result from vitamin K deficiency or the use of anticoagulants that block vitamin K-dependent production of procoagulant factors. These conditions also affect the level of factor VII, an extrinsic pathway factor. Since factor VII has a short half-life relative to the vitamin K-dependent factors of the intrinsic pathway, nutritional or therapeutic vitamin K-dependent factor deficiency can sometimes result in an extended PT with a normal aPTT. Consumption coagulopathies, such as disseminated intravascular coagulation (DIC), can produce an extended aPTT due to depletion of intrinsic factors. The aPTT can also be extended in conditions that reduce the production of procoagulant factors (ie, severe liver disease or malnutrition). Inhibitors, both factor specific and nonspecific, can also prolong the aPTT. A description of the many potential causes of an extended aPTT is described in more detail in the online Coagulation Appendix: Lupus Anticoagulants.
What are the complicating factors for aPTT?
7 The first group of complicating factors encompasses those that affect the bioavailability of heparin . Aging, obesity, changes in heparin binding proteins, hepatic disease, renal disease, and heparin resistance fall under this heading. The second group of complicating factors includes those that alter the aPTT dose response to heparin.
What are the factors that affect the APTT?
The aPTT is sensitive to deficiency or inhibition of factors in the intrinsic pathway. These include the contact factors; high molecular weight kininogen (HMWK), prekallikrein, and factor XII along with procoagulant factors XI, IX, VIII. The aPTT is less sensitive to deficiencies of X, V, prothrombin, and fibrinogen. 1 Nonspecific, lupus-type anticoagulants can also extend the aPTT, but the more sensitive aPTT-LA test should be used to screen for this condition.
What tubes should be collected after a citrate?
Any tube containing an alternative anticoagulant should be collected after the blue-top tube. Gel-barrier tubes and serum tubes with clot initiators should also be collected after the citrate tubes. Please print and use the Volume Guide for Coagulation Testing to ensure proper draw volume.
What is partial thromboplastin time?
Partial Thromboplastin Time, Activated - The aPTT is a screening test that will detect deficiencies or inhibitors to the intrinsic (Factors VIII, IX, XI and XII) and common (Factors II, V, X and fibrinogen) pathway coagulation factors.
What should the fill volume be for a whole blood tube?
Whole blood:The tubes should be at 100% +/- 10% fill volume in order to obtain the correct ratio.
How long to centrifuge platelet-poor plasma?
Platelet-poor plasma:Centrifuge light blue-top tube 15 minutes at approximately 1500 g within 60 minutes of collection. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and place into a plastic vial. Centrifuge a second time and transfer platelet-poor plasma into a new plastic vial. Plasma must be free of platelets (<10,000/mcl). Freeze immediately and ship on dry ice.
How long is a pediatric reference interval?
Flagging not provided. Pediatric reference intervals have not been established. Based on published literature, the adult reference interval (23-32 seconds) is generally applicable down to approximately 6 months of age with younger patients having a slightly higher upper limit by several seconds.
Is Quest Diagnostics a registered trademark?
Quest, Quest Diagnostics, the associated logo, Nichols Institute and all associated Quest Diagnostics marks are the registered trademarks of Quest Diagnostics. All third party marks— ® and ™ — are the property of their respective owners. © 2000-2019 Quest Diagnostics Incorporated. All rights reserved.
What is a PTT?
A PTT may be used to assess patients with signs or symptoms of hemorrhage or thrombosis. For example: abnormal bleeding, hemorrhage or hematoma petechiae or other signs of thrombocytopenia that could be due to disseminated intravascular coagulation; swollen extremity with or without prior trauma.
What is PTT in coagulation?
A PTT may be useful in evaluating patients who have a history of a condition known to be associated with the risk of hemorrhage or thrombosis that is related to the intrinsic coagulation pathway. Such abnormalities may be genetic or acquired. For example: dysfibrinogenemia; afibrinogenemia (complete); acute or chronic liver dysfunction or failure, including Wilson's disease; hemophilia; liver disease and failure; infectious processes; bleeding disorders; disseminated intravascular coagulation; lupus erythematosus or other conditions associated with circulating inhibitors, e.g., Factor VIII Inhibitor, lupus-like anticoagulant, etc.; sepsis; von Willebrand's disease; arterial and venous thrombosis, including the evaluation of hypercoagulable states; clinical conditions associated with nephrosis or renal failure; other acquired and congenital coagulopathies as well as thrombotic states.
What is the purpose of PTT?
The PTT is most commonly used to quantitate the effect of therapeutic unfractionated heparin and to regulate its dosing. Except during transitions between heparin and warfarin therapy, in general both the PTT and PT are not necessary together to assess the effect of anticoagulation therapy. PT and PTT must be justified separately.
Is a thrombolytic test necessary?
Testing prior to any medical intervention associated with a risk of bleeding and thrombosis (other than thrombolytic therapy) will generally be considered medically necessary only where there are signs or symptoms of a bleeding or thrombotic abnormality or a personal history of bleeding, thrombosis or a condition associated with a coagulopathy. Hospital/clinic-specific policies, protocols, etc., in and of themselves, cannot alone justify coverage.
Is PTT necessary for warfarin?
The PTT is not useful in monitoring the effects of warfarin on a patient's coagulation routinely. However, a PTT may be ordered on a patient being treated with warfarin as heparin therapy is being discontinued. A PTT may also be indicated when the PT is markedly prolonged due to warfarin toxicity.