
What is the CPT code for evaluation of AAC devices?
For the initial evaluation—to determine the type of AAC device that may be appropriate for the patient—use one of the following evaluation codes: 92605, Evaluation for prescription of non-speech-generating augmentative and alternative communication device, face-to-face with the patient, first hour; and 92618, each additional 30 minutes.
Where does the money for AAC evaluation come from?
The AAC Evaluation can be funded through a variety of sources including school districts, insurance, and Medicaid/Medicare. 4. How long does it take to learn an AAC system? This is a question that I am often asked because many people have the misconception that once you have a communication system, you can use it right away without any training.
What is an AAC assessment?
All AAC assessments are individualized and differ according to diagnosis, the individual's abilities, communication needs, as well as other individual variables and environmental factors. Prior to submitting a SGD funding request, patients must have a formal evaluation of their cognitive and communication abilities by an SLP.
How much does an AAC device cost?
Clinicians note that traditional AAC devices are bigger, bulkier, and may have added unnecessary components. The costs are substantially different, with AAC devices running $2,000–$4,000 and up; an iPad, for example, costs about $500, and an app around $189.
Does Medicare pay for AAC?
Yes. AAC Assessments and Training Services are covered by Medicare as SLP services if the SLP works in a facility that is a Qualified Provider. Otherwise, SLP services are not covered.
How do I bill an AAC evaluation?
You should use 92507, because you are providing speech-language treatment. You should use 92606 or 92609 only if you are working with the patient on how to use the device itself and/or are modifying or programming it for their use.
How much is a speech generating device?
around $15,000Speech-generating devices typically cost around $15,000. Medicare will cover 80% of the cost. The remaining 20% should be covered by Medicaid and private insurance.
Are AAC devices covered by insurance?
Private insurance may cover the cost of medically necessary AAC devices with a prescription from a medical provider or Speech- Language Pathologist. Medicaid can cover the cost of medically necessary AAC devices with a prescription from a medical provider or Speech-Language Pathologist.
What is the CPT code for AAC device?
The current CPT codes are: 92605, Evaluation for prescription of non-speech-generating augmentative and alternative communication device. 92606, Therapeutic service(s) for the use of non-speech-generating device, including programming and modification.
What is the CPT code for speech therapy evaluation?
Currently, CPT code 92506 is billed for the evaluation of speech, language, voice, communication, and/or auditory processing.
Does Medicare cover speech generating devices?
Speech generating devices are covered if the patient suffers from severe speech impairment and the medical condition warrants the use of a device. Speech generating devices are defined for Medicare coverage purposes to include dedicated speech devices used solely by the individual who has severe speech impairment.
Is an iPad a speech generating device?
The recommended device is the Apple iPad, a speech output communication system.
What is the difference between aided and unaided AAC systems?
AAC systems are diverse: unaided communication uses no equipment and includes signing and body language, while aided approaches use external tools. Aided communication methods can range from paper and pencil to communication books or boards to speech generating devices (SGDs) or devices producing written output.
How long does it take to get an AAC device?
The length of time the process takes depends on the paying source. As a general rule, it may take 30 to 60 days from the date your paperwork was received at AAC Funding.
Are AAC devices FDA approved?
The FDA recognizes AAC devices as medical 'devices' within the 'physical medicine devices intended for human use' category.
How much does TouchChat cost?
TouchChat HD for iPad® / iPod® / iPhone® ($149.99 USD + tax) is a full-featured communication solution for individuals who have difficulty using their natural voice.
Medicare Funding Pages
General Medicare ~ Eligibility ~ SGDs & Accessories ~ Assessments & Training ~ Payment ~ Processes ~ Repairs & Replacements ~ Miscellaneous
General Medicare
Medicare was created by Congress in 1965 and has become the nation's largest health services funding program. Medicare, sometimes called Title XVIII (for the chapter of the Social Security Act in which the Medicare program is codified), operates as a federal health insurance benefits program for:
Eligibility
Medicare regulations state that Durable Medical Equipment will be provided if "the equipment is used in the patient's home or in an institution that is used as a home." In general, this is called a "place of service limitation." Because Medicare classifies SGDs as DME, this limitation applies to SGDs.
Speech Generating Devices and Accessories
Medicare originally adopted 4 "codes" for SGDs, with each code representing a group of devices with similar characteristics. Medicare subsequently changed the codes on two occasions. First, it expanded the number of codes from 4 to 6, and most recently, changed the labels of the codes. The most current codes are listed at the end of this FAQ.
Assessments and Training
Yes. AAC Assessments and Training Services are covered by Medicare as SLP services if the SLP works in a facility that is a Qualified Provider. Otherwise, SLP services are not covered.
Payment
Medicare is a cost reimbursement program, like many insurance policies. This means that the beneficiary must incur a charge -- usually associated with having an examination or procedure performed, or purchasing an item of equipment -- before a claim can be submitted. After the charge is incurred, the claims procedure begins.
Processes
The SLP is the key person in the Medicare claims process related to SGDs. Medicare guidance related to SGDs is unique among all items and medical services Medicare covers in that it designates a non-physician, the SLP, as the primary determiner of a beneficiary's medical The SLP is the key person in the Medicare claims process related to SGDs.
What percentage of Medicare reimbursement is for social workers?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare’s reimbursement rate on average is roughly 80 percent of the total bill. 1. Not all types of health care providers are reimbursed at the same rate. For example, clinical nurse specialists are reimbursed at 85% for most services, while clinical social workers receive 75%. 1.
What is Medicare reimbursement?
Medicare reimburses health care providers for services and devices they provide to beneficiaries. Learn more about Medicare reimbursement rates and how they may affect you. Medicare reimbursement rates refer to the amount of money that Medicare pays to doctors and other health care providers when they provide medical services to a Medicare ...
Is it a good idea to use HCPCS codes?
Using HCPCS codes. It’s a good idea for Medicare beneficiaries to review the HCPCS codes on their bill after receiving a service or item. Medicare fraud does happen, and reviewing Medicare reimbursement rates and codes is one way to help ensure you were billed for the correct Medicare services.
Is speech generating device covered by Medicare?
For a speech generating device (SGD) to be covered by Medicare, it must: be eligible for a defined Medicare benefit category. be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.
Is SGD funding a substitute for AAC?
The SGD funding process is not a substitute for exemplary AAC clinical practice. All AAC assessments are individualized and differ according to diagnosis, the individual's abilities, communication needs, as well as other individual variables and environmental factors.
How often should I bill for a medical evaluation?
Check with your payer when in doubt. In this case, you should consider billing for only one evaluation, even though it spans multiple days. When submitting the claim, wait until you have completed the entire evaluation and bill based on the last date of service you saw the patient for the evaluation.
Can you bill Medicare and Medicaid on the same day?
According to Medicare and Medicaid’s National Correct Coding Initiative (NCCI), which many other payers also follow, the codes may be billed together on the same day—but your documentation must demonstrate that you are providing two distinct and separate services.
Does Medicare reimburse for speech generating devices?
Medica re does not reimburse for the codes specific to evaluation or treatment for non-speech-generating devices . Medicare views these codes as bundled with other services that the SLP would already be performing, such as speech-language evaluation or treatment. For example, Medicare considers the non-speech-generating device evaluation as part ...
What are the changes in the 2020 Audiology payment rate?
Audiologists will generally see minor changes in 2020 payment rates because of two factors: 1) the conversion factor (CF) established by a statutory formula and 2) changes in the practice expense— one of several costs factored into the value of any given procedure code—for audiology codes.
When will audiologist be eligible for MIPS?
Audiologists first became eligible for MIPS in 2019 and will continue to participate in the program in 2020. If an audiologist meets the criteria for a MIPS eligible clinician (EC), they will need to report data associated with quality measures and improvement activities in 2020 that will be used to adjust their payments in 2022.
Why is there no rate established for non-facility services?
Non-Facility: No rate established because service is typically performed in the hospital. If the contractor determines the service can be performed in the non-facility setting, it will be paid at the facility rate.
What is an AAPM?
AAPMs are Medicare approaches that incentivize quality and value. AAPMs take a variety of forms, including accountable care organizations, patient-centered medical homes, bundled payments, and episodes of care. Audiologists have been able to participate in the AAPM option since 2017. Those who successfully participate in 2020 will be eligible to receive a 5% lump-sum incentive payment on their Part B services in 2022. An example of an AAPM is the Medicare Shared Savings Program ACO-Track
Is audiology part of Medicare?
Outpatient audiology services provided under Part B of the Medicare program are paid under the Medicare Physician Fee Schedule (MPFS). Congress approves annual payment updates to the MPFS. Starting in 2020, annual MPFS payment updates are frozen at 0.0% through 2025 because of a provision of the Medicare Access and CHIP Reauthorization Act of 2015. Additional payment adjustments—based on participation in Merit-Based Incentive Payment System (MIPS) or Advanced Alternative Payment Models (AAPMs)—may also apply.
What is ASCQR program?
The Ambulatory Surgical Center Quality Reporting (ASCQR) Program is a pay-for-reporting, quality data program administered by the Centers for Medicare & Medicaid Services (CMS). Under this program, ASCs report quality of care data for standardized measures to not receive a payment penalty to their annual payment update to their ASC annual payment rate.
How to contact ASCQR?
Submit questions and search for answers on the ASCQR Program through the Quality Question and Answer Tool or call the Hospital OQR Support at (866) 800-8756 weekdays from 7 a.m. to 6 p.m. Eastern Time.
Why is ASCQR public?
Data collected through the ASCQR program is publicly reported so people with Medicare and other consumers can find and compare the quality of care provided at ambulatory surgical centers. Publishing these data can improve facility performance by providing benchmarks for selected clinical areas and public view of facility data.
Does CMS continue to evaluate measures?
CMS continues to evaluate measures, ensuring meaningful information is collected to ensure quality of care, removing measures that are no longer needed and adding measures to continue the quality improvement process.
What is AAC specialist?
There are speech-language pathologists that are AAC specialists in all different settings including clinics, schools, day programs, and universities. To seek a specialist in your area, reach out to either your school district or your child’s therapists who will be able to provide you with a recommendation.
How long does it take to learn AAC?
AAC is like a second language and can take months or years to learn well. Although it takes time to learn, once learned, a communication system can change the life of a child with complex communication needs. I have seen this transformation over and over again with my clients for 18 years, which is what gravitated me towards the field of AAC.
Does AAC help with speech?
AAC does not hinder speech. There has been substantial research that has shown that AAC helps children develop speech. For recent research on this topic, check out an article written by Diane C. Millar, Janice C. Light, and Ralf W. Schlosser. To learn more about the myths of AAC, click here. 6.
How Do We Define Nursing Facilities?
These types of facilities may include skilled nursing facilities (SNFs), nursing facilities (NFs), or rehabilitation centers. The key is that they provide skilled nursing to people who need medical care, rehabilitation care, or long-term nursing care. They may stand along facilities or affiliated with a hospital.
Medicaid and Medicare: What is the Difference?
Medicaid is a federal and state program for people with limited income. If someone receives Supplemental Security Income (SSI), they will be covered by Medicaid. Medicaid will also cover people who receive waiver funding for home and community-based services (HCBS).
What Counts as Durable Medical Equipment?
AAC that counts as DME may include devices that use a recorded voice (digitized speech) or a computerized voice (synthesized speech). These devices may use different types of message formulation, i.e., text to speech, symbol-based communication, or both.
What Does Medicare cover?
Medicare does not cover many types of DME in nursing facilities. If it is labeled as DME, it will not be covered. Medicare rules state that DME is for use in a “patient’s home.” And Medicare does not consider a nursing facility to be a patient’s true home. This applies to SNFs and other facilities that provide skilled nursing care.
What Does Medicaid Cover?
Too often, SLPs are told that AAC is not covered by Medicaid in nursing facilities. This is not true. Medicaid covers AAC devices in multiple settings, including nursing facilities (SNFs and NFs). The confusion may stem from the definition of DME, which does not crossover to apply to Medicaid.
Further Barriers to AAC Use in Nursing Facilities
Another potential barrier is a lack of knowledge among the speech pathologists working in these facilities. Graduate programs often do not center AAC and frequently do not offer robust coursework on the topic.
Consider the Tools You Already Have
Don’t forget to look at the technology a patient may already have. Do they own a smartphone? Or an iPad? Perhaps an iPad Pro? You might be able to use the accessibility settings on the device to support their communication needs. For instance, you can turn the Notes app on an iPhone into an on-the-spot text to speech device:
Who Qualifies?
- Medicare now classifies SGDs as "durable medical equipment," and they are available to Medicare beneficiaries when the following four criteria are met:
What Is The RMRP Policy?
- Medicare has issued a Regional Medical Review Policy (RMRP) on Speech Generating Devices (SGDs) that identifies the required components of the SLP evaluation and report. View a complete copy of the RMRP.
What Is The AAC Assessment / Application Protocol?
- This SGD Assessment Protocolis intended as a guide so that speech-language pathologists will conduct complete assessments and prepare written reports that address all of the points identified in the RMRP.
Who Can Conduct The Assessment?
- The RMRP requires that a speech-language pathologist holding a Certificate of Clinical Competence issued by the American Speech-Language-Hearing Association conduct the assessment for an SGD.
Can The Assessment Be reimbursed?
- Yes. Medicare has established procedure codes and reimbursement rates for SGD assessments and devices. However, in order to be reimbursed, the SLP must meet the requirements to be a provider of Medicare speech-language pathology services.
Must A Written Report Be Prepared?
- Yes. The SLP report, consistent with the RMRP, must be completed, and then sent to the beneficiary's doctor for review. A doctor's prescription is needed to obtain reimbursement for the recommended SGD and any software and accessories. This Assessment /Application Protocol identifies the specific topics to be addressed in the report.
Is Additional Help available?
- Yes. SLPs with questions about the SGD Assessment Protocol may contact members of the Medicare Implementation Team. Contact information is listed at the end of the Protocol. To obtain more information about Medicare coverage of SGDs, go to "Frequently Asked Questions."
Reference Information
- The information on the site was developed and copyrighted by members of the Medicare Implementation Team. The site is partially supported by the National Institute on Disability and Rehabilitation Research (NIDRR). If you would like to link to or reference material on this site, please follow the reference instructions. © 2001-2011 Medicare Implementation Team. All right…
General Medicare
Eligibility
- Will Medicare Provide SGDs to Residents of Nursing Homes or other Types of Assisted Living Ar…
Medicare regulations state that Durable Medical Equipment will be provided if "the equipment is used in the patient's home or in an institution that is used as a home." In general, this is called a "place of service limitation." Because Medicare classifies SGDs as DME, this limitation applies t… - Will Medicare Reimburse for SGDs For Individuals Receiving Hospice Services? 11/20/04
There are two types of hospice care: residential and in-home. A residential hospice offers a setting where the individual receives hospice care but also serves as the person's residence. As an alternative, hospice care also can be provided as a constellation of services provided to an in…
Speech Generating Devices and Accessories
- What SGDs Are Covered by Medicare? 11/20/04
Medicare originally adopted 4 "codes" for SGDs, with each code representing a group of devices with similar characteristics. Medicare subsequently changed the codes on two occasions. First, it expanded the number of codes from 4 to 6, and most recently, changed the labels of the codes. … - Why Aren't All SGDs Covered? 11/20/04
Medicare will cover all dedicated devices and computer-based and PDA-based devices "that have been modified to run only AAC software. " Medicare's coverage guidance on SGDs: the Regional Medical Review Policy (RMRP) and the National Coverage Decision on SGDs (# 60-23), state tha…
Assessments and Training
- Are AAC Assessments and Training -- SLP Services -- Covered? 11/20/04
Yes. AAC Assessments and Training Services are covered by Medicare as SLP services if the SLP works in a facility that is a Qualified Provider. Otherwise, SLP services are not covered. Typically, the setting the SLP works in determines whether or not he/she is "Medicare Qualified" to be reim… - How Much Will Medicare Pay SLPs for AAC Assessments and Training? 11/23/04
If an SLP works in a Medicare Qualified setting and thus is a "Qualified Provider," Medicare will pay for an SGD Evaluation and for SGD Training. There are 3 CPT codes that address these activities: Back to FAQ Table of Contents
Payment
- What Does "Accept Assignment" Mean? 11/20/04
Medicare is a cost reimbursement program, like many insurance policies. This means that the beneficiary must incur a charge -- usually associated with having an examination or procedure performed, or purchasing an item of equipment -- before a claim can be submitted. After the cha… - What If A Beneficiary Cannot Afford the Co-Payment? Can A Co-Payment Be Waived? Must it be …
Medicare requires durable medical equipment suppliers to collect the 20 % co-payment -- of either the actual charge for the device, or of the fee schedule amount -- from beneficiaries. However, as the cost of items increases, beneficiaries' ability to afford the co-payment amount can become …
Processes
- What is the SLP's Role in Medicare Funding of SGDs? 11/20/04
The SLP is the key person in the Medicare claims process related to SGDs. Medicare guidance related to SGDs is unique among all items and medical services Medicare covers in that it designates a non-physician, the SLP, as the primary determiner of a beneficiary's medical The SL… - What is the Physician's Role in Medicare Funding of SGDs? 11/20/04
The physician is a necessary part of the Medicare claims process. No Medicare payment will be made for an SGD, AAC software, or accessory without a physician's prescription. Medicare has not required that any particular physician prepare the prescription. Thus, Medicare beneficiaries …
Repairs and Replacements
- Are SGD and Accessories Repairs Covered? 11/20/04
Medicare will cover SGD and accessory repairs -- both parts and labor -- for devices and accessories, which are beyond their warranty periods. During the warranty period, it is expected the supplier will be responsible for repairs. Beyond that time, Medicare will cover SGD and acces… - What if my device cannot be repaired? 11/20/04
Medicare assumes that durable medical equipment will have a useful life of 5 years. This means that Medicare will not replace items of durable medical equipment within a five-year span, except when a substitution request is based on change of beneficiary condition. The impacts of this pra…
Miscellaneous
- How Many People Have Benefitted From the Medicare Policy Change for SGD? 03/26/2012
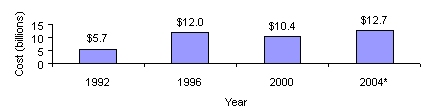
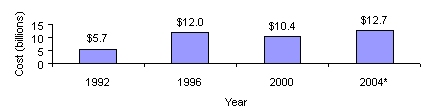
Medicare's policy change for Speech Generating Devices (SGDs) has had a profound positive impact on Medicare beneficiaries, and on persons who receive health benefits from other funding programs. Table 1 reports the number of SGDs Medicare has approved and purchased in the 10 …
Introduction
- Pursuant to EB 36-2002, an ASHA Ad Hoc Speech-Generating Devices (SGD) Committee was formed and charged with the responsibility to a) pilot and refine an SGD reimbursement protocol; b) make recommendations for a variety of educational opportunities focusing on Medicare SGD coverage and documentation; c) develop a proposal for a mentoring program for speech-langua…
Medicare Funding of Sgds
- The ASHA SGD Committee developed a checklist to assist an SLP in the completion of a SGD funding Request. The SLP Checklist stems from the Regional Medical Review Policy (RMRP) (see Appendix A) issued by Medicare. The items on the checklist reflect the required components of the SLP report for funding by Medicare. SLPs should be aware that when any one of the items in …
SLP Checklist
- Introduction
1. For a speech generating device (SGD) to be covered by Medicare, it must: 1.1. be eligible for a defined Medicare benefit category 1.2. be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member 1.3. me… - Instructions for Use
Respond to each of the questions posed in the following grid to indicate whether the SGD funding report contains all of the items to ensure coverage and payment by Medicare. Check "yes" when you have completed or identified the element in the funding report prior to forwarding the reques…
SGD Recommendations
- Recommendations for a variety of educational opportunities focusing on SGD coverage and documentation.
Medicare SGD Funding—Internet Resources
- American Speech-Language-Hearing Association (ASHA) 1. Durable Medical Equipment Regional Carriers (DMERCs) policies on SGDs 2. Coverage Policy on Speech-Generating Devices AAC Institute 1. Funding a Speech-Generating Device: What You Need To Know 2. How to Support Your Request for a SGD 3. Requirements for a Funding Request for a SGD AAC Rehabilitation Enginee…