
How do you qualify for QMB program?
What is a Qualified Medicare Beneficiary (QMB) Program? The QMB program is a state program that helps covers the cost of Medicare premiums, deductibles and coinsurance that Medicare beneficiaries usually pay. You may be eligible for the QMB program if you are entitled to Medicare Part A coverage, and have limited income and resources.
What is the income limit for QMB?
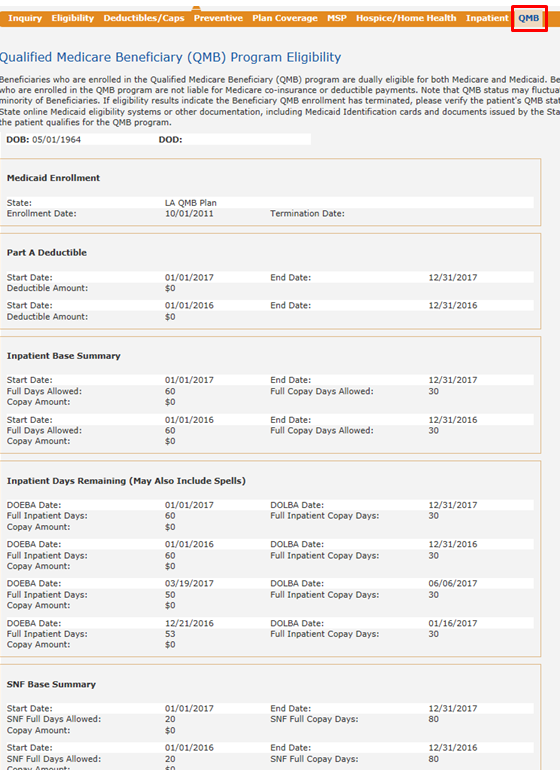
Qualified Medicare Beneficiary (QMB) is a Medicaid program for people who are already receiving Medicare benefits. The purpose of the program is to reduce the cost of medications and copays for doctors, hospitals, and medical procedures. Important Note: The QMB program may differ by state.
Do QMB patients have copays?
Sep 15, 2021 · The Qualified Medicare Beneficiary program is a type of Medicare Savings Program (MSP). The QMB program allows beneficiaries to receive financial help from their state of residence with the costs of Medicare premiums and more. A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays.
Can We Bill QMB patients?
Feb 08, 2022 · The Qualified Medicare Beneficiary (QMB) Program is designed to assist your mother by paying her: Medicare Part B premium; Medicare Part B premiums are based upon the income your mother reported on her taxes 2 years ago. Her premium can range from $144.60 to $491.60 per month (as of 2020), depending on her reported income.

What does QMB mean on Medicare?
Qualified Medicare BeneficiaryIf you're among the 7.5 million people in the Qualified Medicare Beneficiary (QMB) Program, Medicare providers aren't allowed to bill you for services and items Medicare covers, including deductibles, coinsurance, and copayments. If a provider asks you to pay, that's against the law.May 15, 2020
What is a QMB only plan?
QMB Only is a program that ONLY provides financial assistance for certain Medicare costs. It does not provide any additional Medicaid coverage, and cannot be used to receive benefits not covered by Medicare.
What does Medicare beneficiary pay?
The Qualified Medicare Beneficiary (QMB) Program is one of the four Medicare Savings Programs that allows you to get help from your state to pay your Medicare premiums. This Program helps pay for Part A premiums, Part B premiums, and deductibles, coinsurance, and copayments.
Does Social Security count as income for QMB?
An individual making $1,800 from Social Security cannot qualify for QMB because they are over the $1,133 income limit.
What does Ahcccs QMB only cover?
AHCCCS QMB – ONLY is Medicare Savings Program that pays Medicare Part A premium (when applicable) and Medicare Part B premium. Claim payments are limited to Medicare deductible, coinsurance, and copay when Medicare pays first. Claims are normally crossed over by Medicare to the AHCCCS Administration.
What is maximum out-of-pocket for Medicare?
The US government sets the standard Medicare Advantage maximum out-of-pocket limit every year. In 2019, this amount is $6,700, which is a common MOOP limit. However, you should note that some insurance companies use lower MOOP limits, while some plans may have higher limits.Oct 1, 2021
Which Medicare Parts require additional premiums from beneficiaries?
Medicare Advantage plan enrollees generally pay the monthly Part B premium and many also pay an additional premium directly to their plan. Medicare Advantage plans are required to place a limit on beneficiaries' out-of-pocket expenses for Medicare Part A and Part B covered services ($6,700 in 2015).Mar 20, 2015
Do all Medicare recipients pay a premium?
Most people don't pay a Part A premium because they paid Medicare taxes while working. If you don't get premium-free Part A, you pay up to $499 each month. If you don't buy Part A when you're first eligible for Medicare (usually when you turn 65), you might pay a penalty.
What are the eligibility requirements for QMB?
Although the rules may vary from state to state, in general, you must meet the following requirements in order to be eligible for the QMB program: You must be entitled to Medicare Part A. Your income must be at or below the national poverty level (income limits generally change annually).
How to contact Medicare.org?
Call us at (888) 815-3313 — TTY 711 to speak with a licensed sales agent.
Does QMB cover Medicare?
It means that your state covers these Medicare costs for you, and you have to pay only for anything that Medicare normally does not cover. QMB does not supplement your Medicare coverage but instead ensures that you will not be precluded from coverage because you cannot afford to pay the costs associated with Medicare.
What is a qualified Medicare beneficiary?
The Qualified Medicare Beneficiary program is a type of Medicare Savings Program (MSP). The QMB program allows beneficiaries to receive financial help from their state of residence with the costs of Medicare premiums and more. A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. If you’re a Medicare beneficiary, you know that health care costs can quickly add up. These costs are especially noticeable when you’re on a fixed income. If your monthly income and total assets are under the limit, you might be eligible for a Qualified Medicare Beneficiary program, or QMB.
What is QMB insurance?
The QMB program pays: The Part A monthly premium (if applicable) The Part B monthly premium and annual deductible. Coinsurance and deductibles for health care services through Parts A and B. If you’re in a QMB program, you’re also automatically eligible for the Extra Help program, which helps pay for prescription drugs.
How much money do you need to qualify for QMB?
To be eligible for a QMB program, you must qualify for Part A. Your monthly income must be at or below $1,084 as an individual and $1,457 as a married couple. Your resources (money in checking and/or savings accounts, stocks, and bonds) must not total more than $7,860 as an individual or $11,800 as a married couple.
Can QMB members pay for coinsurance?
Providers can’t bill QMB members for their deductibles , coinsurance, and copayments because the state Medicaid programs cover these costs. There are instances in which states may limit the amount they pay health care providers for Medicare cost-sharing. Even if a state limits the amount they’ll pay a provider, QMB members still don’t have to pay Medicare providers for their health care costs and it’s against the law for a provider to ask them to pay.
Does Medicare Advantage cover dual eligibility?
A Medicare Advantage Special Needs Plan for dual-eligible individuals could be a fantastic option. Generally, there is a premium for the plan, but the Medicaid program will pay that premium. Many people choose this extra coverage because it provides routine dental and vision care, and some come with a gym membership.
Is Medigap coverage necessary for QMB?
Medigap coverage isn’t necessary for anyone on the QMB program. This program helps you avoid the need for a Medigap plan by assisting in coverage for copays, premiums, and deductibles. Those that don’t qualify for the QMB program may find that a Medigap plan helps make their health care costs much more predictable.
What is QMB in Medicare?
The Qualified Medicare Beneficiary (QMB) program is a state program to help people with lower income pay for out-of-pocket Medicare expenses, such as deductibles, co-payments and premiums .
When is QMB updated?
These figures are usually updated in April of each year and can be found in the Federal Register, the official government source for administrative changes.
Where to apply for QMB in Maryland?
You can request an application for QMB at your local health department, doctor's office, or hospital social work department. Applications may be downloaded from the Maryland Department of Health website. You can apply in person or by mailing the application to your local department of social services.
How does Medicaid QMB work?
In addition to covering Medicare premiums for eligible QMB recipients, one of the benefits of the QMB program is having protection from improper billing. Improper billing refers to when health care providers inappropriately bill a beneficiary for deductibles, copayments or coinsurance.
Who is eligible for QMB?
You must be eligible for both Medicare and Medicaid to be eligible for QMB benefits. While Medicare’s eligibility requirements are federally mandated, each state may set its own qualifying restrictions for Medicaid.
What are other Medicare and Medicaid assistance programs?
QMB is not the only program available to dual-eligible beneficiaries. Others include:
Topics on This Page
See more on peoples-law.org
What Is The Qualified Medicare Beneficiary Program (Qmb)?
- The Qualified Medicare Beneficiary (QMB) program is a state program to help people with lower income pay for out-of-pocket Medicare expenses, such as deductibles, co-payments and premiums. Read the regulations: Code of Md. Regulations 10.09.24.03-3; Code of Federal Regulations, Title 42 § 400.200 Read the law: U.S. Code, Title 42, Chapter 7, Subtitle XIX
Eligibility
- Individuals or couples must: 1. qualify to receive Medicare Part A, even if not enrolled 2. NOT be financially eligible for Medical Assistance 3. have limited income and assets There are additional non-financial requirements. Note that QMB is not a program for families. Read the regulations: Code of Md. Regulations 10.09.24.03-3 Income and Assets - Individuals or married …
Applying
- You can request an application for QMB at your local health department, doctor's office, or hospital social work department. Applications may be downloaded from the Maryland Department of Health website. You can apply in person or by mailing the application to your local department of social services.
Appeals
- Any denial, termination, or reduction of benefits can be appealed. Call the telephone number provided in the denial letter you receive. Or call 1-800-332-6347 to request a hearing. File appeals in writing at your local Department of Social Services office. It is best to file in person and to get a receipt showing that you filed the appeal. Keep in mind: 1. Appeals must be filed within 90 days …