Full Answer
What is the hospital VBP program?
The Hospital VBP Program rewards acute care hospitals with incentive payments for the quality of care provided in the inpatient hospital setting. This program adjusts payments to hospitals under the Inpatient Prospective Payment System (IPPS) based on the quality of care they deliver. Why is the Hospital VBP Program important?
What is Hospital Value-Based Purchasing (VBP)?
The Hospital Value-Based Purchasing (VBP) Program is part of our ongoing work to structure Medicare’s payment system to reward providers for the quality of care they provide. This program adjusts payments to hospitals under the Inpatient Prospective Payment System (IPPS), based on the quality of care they deliver.
What does VBP stand for?
Value-Based Purchasing (VBP) Linking provider payments to improved performance by health care providers. This form of payment holds health care providers accountable for both the cost and quality of care they provide. It attempts to reduce inappropriate care and to identify and reward the best-performing providers. Back to Glossary Index.
What is the hhvbp model?
The HHVBP Model is designed to give Medicare-certified home health agencies (HHAs) incentives to give higher quality and more efficient care. When does the HHVBP Model start?

What is VBP Medicare?
The Hospital Value-Based Purchasing (VBP) Program is part of our ongoing work to structure Medicare's payment system to reward providers for the quality of care they provide. This program adjusts payments to hospitals under the Inpatient Prospective Payment System (IPPS), based on the quality of care they deliver.
What is HAC medical term?
Hospital-Acquired Conditions (HACs) are conditions that a patient develops while in the hospital being treated for something else. These conditions cause harm to patients.
What is PSI and Hac?
The HAC Reduction Program is comprised of patient safety indicator (PSI) 90 (The Patient Safety and Adverse Events Composite), as well as healthcare-associated infections (HAI). PSI 90 was developed by the Agency for Healthcare Research and Quality (AHRQ) and is used to track potential complications and adverse events.
What is a HAC score?
A Hospital's Total HAC Score is defined by CMS as the sum of weighted Domain 1 and Domain 2 scores. For FY15 - FY 17, the Total HAC Score ranges from 1-10. Beginning in FY18, CMS changed the scoring methodology for the HAC Reduction Program. Under this revised methodology, scores tend to range between -3 and 3.
What is an example of HAC?
For instance, if a patient falls out of bed while in a hospital, the consequent broken hip was not present on admission, so the "complication" of "broken hip" would be demoted as a "Falls and trauma" HAC.
How is the HAC POA program different from the HAC reduction program?
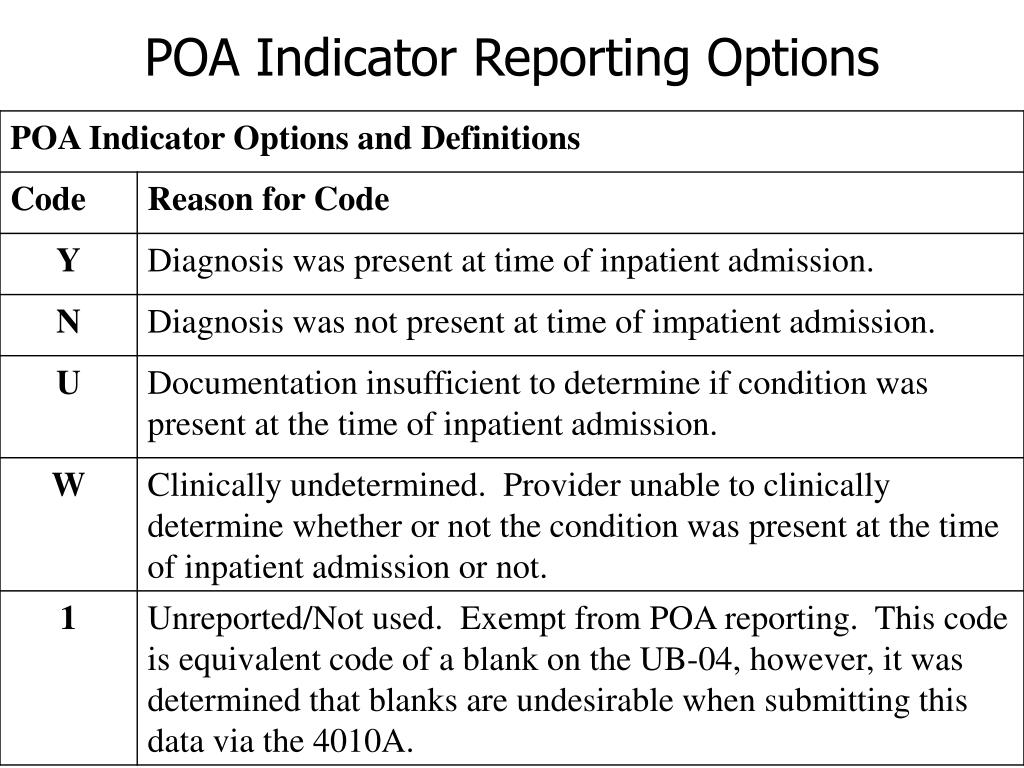
How is the HAC POA program different from the HAC reduction program? The HAC POA program indicates any conditions that are present upon admission. To contrast, the HOA Reduction Program aims to reduce hospital acquired conditions by reducing all HOA payments by 1 percent.
What is HAC payment?
The Hospital-Acquired Condition (HAC) Reduction Program is a value-based-purchasing program for Medicare that supports the Centers for Medicare and Medicaid Services' (CMS') long-standing effort to link Medicare payments to healthcare quality in the inpatient hospital setting.
What is a PSI healthcare?
Patient Safety Indicators (PSIs), developed by the federally operated Agency for Healthcare Research and Quality (AHRQ), are specifically intended to measure the occurrence rate of potentially preventable complications or adverse events that patients experience during their hospital stays.
What is PSI medical term?
The Patient Safety Indicators (PSIs) are a set of 26 indicators (including 18 provider-level indicators) developed by the Agency for Healthcare Research and Quality (AHRQ) to provide information on safety-related adverse events occurring in hospitals following operations, procedures, and childbirth.
Does Medicare pay for hospital-acquired conditions?
Starting in 2009, Medicare, the US government's health insurance program for elderly and disabled Americans, will not cover the costs of “preventable” conditions, mistakes and infections resulting from a hospital stay.
What are the hospital-acquired infections?
Hospital-acquired infections are caused by viral, bacterial, and fungal pathogens; the most common types are bloodstream infection (BSI), pneumonia (eg, ventilator-associated pneumonia [VAP]), urinary tract infection (UTI), and surgical site infection (SSI).
What are the value based purchasing measures?
Linking provider payments to improved performance by health care providers. This form of payment holds health care providers accountable for both the cost and quality of care they provide. It attempts to reduce inappropriate care and to identify and reward the best-performing providers.
What is VBP in Medicare?
The Hospital Value-Based Purchasing (VBP) Program is part of our ongoing work to structure Medicare’s payment system to reward providers for the quality of care they provide. This program adjusts payments to hospitals under the Inpatient Prospective Payment System (IPPS), based on the quality of care they deliver.
What is the VBP program?
The hospital VBP Program rewards acute care hospitals with incentive payments based on the quality of care they provide, rather than just the quantity of services they provide. The statutory requirements of the Hospital VBP Program are set forth in Section 1886 (o) of the Social Security Act.
What is the VBP report for FY 2021?
The FY 2021 Hospital VBP Program Percentage Payment Summary Report gives hospitals their Total Performance Score and value-based incentive payment percentage that will be applied to each Medicare fee-for-service patient discharge in FY 2021.
When was the ECE issued for VBP?
On August 26, 2020, we issued the COVID-19 IFC, which amended the Extraordinary Circumstance Exception (ECE) announced for the Hospital VBP Program in a press release dated March 22, 2020, and a guidance memo (PDF) issued March 27, 2020. CMS has granted exceptions and extensions for certain deadlines under its ECE policy to assist health care ...
Why did CMS grant exceptions and extensions?
In some instances, CMS granted the exceptions and extensions because the provider’s response to COVID-19 may greatly impact collected data and that data should not be considered in a CMS quality reporting or pay-for-performance program.
What is HAC reduction?
What is the Hospital-Acquired Condition (HAC) Reduction Program? The HAC Reduction Program encourages hospitals to improve patients’ safety and reduce the number of conditions people experience from their time in a hospital, such as pressure sores and hip fractures after surgery.
What hospitals are exempt from HAC?
Some hospitals and hospital units, such as the following, are exempt from the HAC Reduction Program: Critical access hospitals. Rehabilitation hospitals and units.
Why is HAC reduction important?
Why is the HAC Reduction Program important? The HAC Reduction Program encourages hospitals to improve patients’ safety and implement best practices to reduce their rates of infections associated with health care.
Is Maryland exempt from HAC reduction?
Maryland hospitals are exempt from payment reductions under the HAC Reduction Program because they currently operate under a waiver agreement between CMS and the state of Maryland.
When does the HHVBP Model start?
On January 1, 2016, we’ll implement the HHVBP Model in all Medicare-certified HHAs in nine states that represent each geographic area of the nation: Arizona, Florida, Iowa, Maryland, Massachusetts, Nebraska, North Carolina, Tennessee, and Washington.
How will the Model work?
We’ll adjust payments to HHAs for services based on the quality of care, not just quantity of the services they provide in a given performance period. Also, the Model will test whether larger incentives for giving better quality care can make better outcomes from home health services.
What do HHAs in the HHVBP Model need to do to get started?
If your HHA is provides services in one of the nine states in the HHVBP Model, we encourage you to:
What is a VBP?
The Hospital Value-Based Purchasing (VBP) Program adjusts hospital inpatient Medicare payments based off performance on a set of quality and efficiency measures. It is one of three mandatory pay-for-performance (P4P) programs that the Affordable Care Act introduced and is managed by the Center for Medicare and Medicaid Services (CMS). VBP promotes quality care delivery, positive patient experience, and cost effectiveness by factoring each of these elements into scoring. Like the other P4P programs, low-scoring hospitals see lower reimbursement rates, but VBP is the only program in which high-scoring hospitals see an increase in their Medicare reimbursements, resulting in a net neutral effect on the budget.
What is the impact of VBP?
For example, VBP measures Medicare spending per beneficiary performance, which also impacts other risk-based payment programs like Medicare Shared Savings. In addition, strong performance on infection measures leads to positive scores for the VBP and HAC Reduction Program. Advisory Board research also indicates that in an emerging retail market, successful hospitals and health systems must offer cost-competitive, high-quality services – both of which VBP directly promotes.
What is a VBP bonus?
Although some policy analysts are critical of the program’s relatively minor financial impact compared to other P4P programs, analysis of annual VBP data indicates that bonuses can be an effective way of offsetting penalties levied in the Readmissions Reduction Program and Hospital-Acquired Conditions ( HAC) Reduction Program.
Does VBP increase Medicare reimbursement?
Like the other P4P programs, low-scoring hospitals see lower reimbursement rates, but VBP is the only program in which high-scoring hospitals see an increase in their Medicare reimbursements, resulting in a net neutral effect on the budget. Download the Cheat Sheet.
What is a VBP?
VBP is a catchall term for ACOs and other modes for restructuring healthcare around a system that puts more weight on quality metrics or the aggregate health of a population rather than how many visits someone makes to the hospital or how many procedures one has.
How to implement VBP?
To prepare for a successful VBP implementation, healthcare facilities and coders should consider doing the following: 1 Create a multidisciplinary team to ensure thorough oversight of hospital-acquired conditions and other issues relating to changing reimbursement. 2 Adopt best practices through nationally recommended evidence-based medicine practice guidelines and monitor compliance. 3 Take action based on data outcomes to protect patients, reduce adverse events, and increase efficiency. 4 Perform patient population-level analysis of HCCs and RAFs. 5 Educate physicians about how their care decisions and documentation will impact reimbursement. Include education on:#N#Documenting diagnoses for HCCs and other value-based programs.#N#Thinking beyond medical necessity; encourage documentation of all comorbid conditions, documentation of manifestations due to an underlying etiology, and documentation of wellness measures such as screenings, interventions, and social determinants.#N#Ensuring timely and ongoing education regarding VBP model changes associated with coding and reimbursement requirements.#N#Reviewing claims data prior to submission to ensure documentation meets standards and coding is based on documentation.#N#Performing periodic clinical documentation and coding reviews including post audit education with staff and physicians.
What is the Affordable Care Act?
The Affordable Care Act is promoting the use of ACOs and levies penalties for hospital readmissions to encourage better follow-up care outside the hospital. It is a more data-driven vision of healthcare reform that not only improves quality and efficiency but also reduces costs.
How are VBPs calculated?
VBPs are calculated by using numerous measures of quality and determining the overall health of populations. Unlike the traditional FFS model, value-based care is driven by data; providers must report to the Centers for Medicare & Medicaid Services (CMS) on specific metrics and demonstrate improvement.
What is a VBP model?
Under a VBP model, primary, specialty, and acute care specialties are integrated and healthcare providers work as a networked team to deliver the best-coordinated care.
Who is Viola Apostoli?
Viola Apostoli, CPC, CEMC, CRC, began her career as a medical biller in a small level 1 trauma and teaching community hospital in Ohio over 12 years ago. She worked as a facility coder; however, most of her experience entails providing coding and billing services to physician practices in freestanding and provider-based settings. Apostoli has played an important role in provider education as well as educating the office staff in coding and billing matters. She has assisted physician practices in a variety of specialties in new service lines, as well as her team in learning new systems such as value-based payments and risk adjustment. Apostoli continues to conduct provider audits, coder audits, and provider education, as well as staff education on a variety of topics.
