
Mandated benefits (also known as “mandated health insurance benefits” and “mandates”) are benefits that are required to cover the treatment of specific health conditions, certain types of healthcare providers, and some categories of dependents, such as children placed for adoption.
Full Answer
What is the Medicare mandatory claim submission rule?
The term Medicare beneficiary identifier (Mbi) is a general term describing a beneficiary's Medicare identification number. For purposes of this manual, Medicare beneficiary identifier references both the Health Insurance Claim Number (HICN) and the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
Do I have to file Medicare claims?
Physicians and suppliers are not required to file claims on behalf of Medicare beneficiaries for: • Used Durable Medical Equipment (DME) purchased from a private source; • Medicare Secondary Payer (MSP) claims when you do not possess all the information necessary to file a claim; • Foreign claims (except in certain limited situations);
What are initial claims in Medicare?
Mandatory Claim Submission. Section 1848 (g) (4) of the Social Security Act requires that you submit claims for all your Medicare patients for services rendered. This requirement applies to all physicians and suppliers who provide covered services to Medicare beneficiaries. Providers may not charge patients for preparing or filing a Medicare claim.
What is Medicare and is it mandatory?
Feb 04, 2022 · Reminder on mandatory Medicare claim submission requirements. The Social Security Act ( Section 1848 (g) (4)) requires that claims be submitted for all Medicare patients. This requirement applies to all physicians and suppliers who provide covered services to Medicare beneficiaries.
What claim form is used for Medicare?
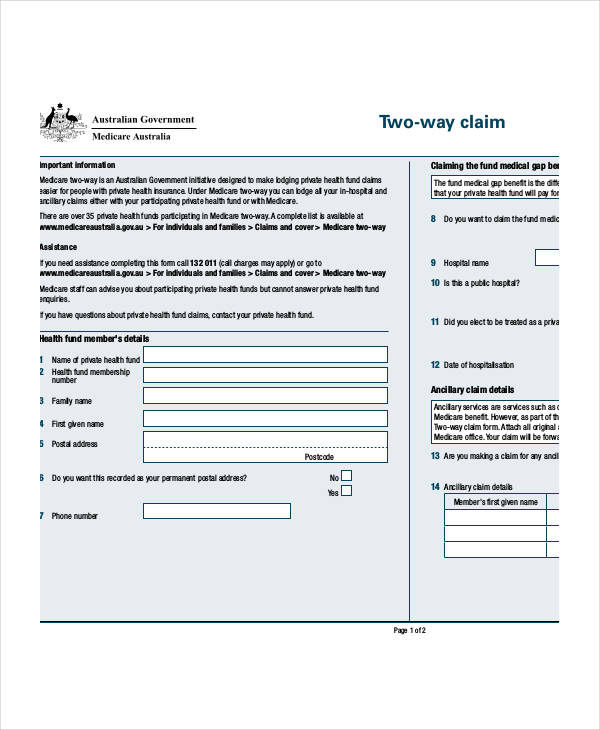
Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB).
What is meant by mandatory filing in regards to Medicare?
Under the Mandatory Claim Submission rule, it is a requirement that providers and suppliers submit Medicare claims for all covered services on behalf of Medicare beneficiaries.May 26, 2021
What is an 837 claim?
An 837 file is an electronic file that contains patient claim information. This file is submitted to an insurance company or to a clearinghouse instead of printing and mailing a paper claim. • The data in an 837 file is called a Transaction Set.
What is a 323 claim?
✓ 323: Interim bill — continuing claim. ✓ 324: Interim bill — final claim. • 34X: Home Health — Services not under a plan of. treatment. ✓ 341: Inpatient admit through discharge claim.
What are Medicare claims?
A Medicare claim is an application for reimbursement from the Australian Government Department of Human Services.
How do I submit a secondary claim to Medicare?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.Sep 9, 2021
What is the difference between an 835 and an 837?
When a healthcare service provider submits an 837 Health Care Claim, the insurance plan uses the 835 to help detail the payment to that claim. The 837-transaction set is the electronic submission of healthcare claim information.Aug 19, 2019
What is an 835 and 837 file?
The X12 837 and 835 files are industry standard files used for the electronic submission of healthcare claim and payment information. The 837 files contain claim information and are sent by healthcare providers (doctors, hospitals, etc) to payors (health insurance companies).
What is an 835 claim?
An 835 is also known as an Electronic Remittance Advice (ERA). It is the electronic transaction that provides claim payment information and documents the EFT (electronic funds transfer). An 835 is sent from insurers to the healthcare provider.
What is revenue code 456?
Revenue Code 456 – Emergency Level II – Must be billed with corresponding CPT codes 99282 or 99283. Revenue Code 451 – Non-emergency/Screening Level – Must be billed with CPT code 99281. Billing Changes for Observation Claims.Jun 3, 2004
What is type of bill 34X?
DME, orthotic, and prosthetics can be billed as a home health service or as a medical and other health service on bill types 32X, 33X, and 34X as appropriate.Jan 1, 2010
What is revenue code 581?
Licensed Practical Nurse (LPN) 581.
What is a claim in Medicare?
Claim is for services initially paid by a third-party insurer who then files a Medicare claim to recoup what Medicare pays as primary insurer (for example, indirect payment provisions); Claim is for other unusual services, which are evaluated by MAC s on a case-by-case basis;
What is Medicare initial claim?
Initial claims are those claims submitted to a Medicare fee-for-service carrier, DME Medicare Administrative Contractor, or FI for the first time, including resubmitted previously rejected claims, claims with paper attachments, demand bills, claims where Medicare is secondary, and non-payment claims. Initial claims do not include adjustments or claim corrections submitted to FI s on previously submitted claims or appeal requests.
What is the 1848 G 4 requirement?
Section 1848 (g) (4) of the Social Security Act requires that you submit claims for all your Medicare patients for services rendered. This requirement applies to all physicians and suppliers who provide covered services to Medicare beneficiaries.
What is the False Claims Act?
False Claims Act. Prohibits knowingly filing a false or fraudulent claim for payment to the government, knowingly using a false record or statement to obtain payment on a false or fraudulent claim paid by the government, or conspiring to defraud the government by getting a false or fraudulent claim allowed or paid.
Do providers have to submit Medicare claims?
Providers who are eligible to enroll in Medicare must do so if he/she provides covered services to a Medicare beneficiary. Under the Mandatory Claim Submission rule, it is a requirement that providers and suppliers submit Medicare claims for all covered services on behalf of Medicare beneficiaries.
What does it mean when a doctor accepts Medicare?
When your doctor accepts Medicare assignment, it also means she or he agrees not to bill you for more than the Medicare deductible and/or coinsurance. Private insurance companies contracted with Medicare may bill Medicare differently.
Can you appeal a Medicare Advantage plan?
If you have prescription drug coverage–whether it’s through a stand-alone Medicare Part D Prescription Drug Plan, or through a Medicare Advantage Prescription Drug plan–and your plan doesn’t cover a drug prescribed for you , you can file an appeal to get your plan to cover the prescription drug or to get it at a lower cost.
What is Medicare Part A?
Medicare is a public health insurance program designed for individuals age 65 and over and people with disabilities. The program covers hospitalization and other medical costs at free or reduced rates. The hospitalization portion, Medicare Part A, usually begins automatically at age 65. Other Medicare benefits require you to enroll.
What happens if you don't sign up for Medicare?
If you choose not to sign up for Medicare Part A when you become eligible, a penalty may be assessed. This penalty depends on why you chose not to sign up. If you simply chose not to sign up when you were first eligible, your monthly premium — if you have to pay one — will increase by 10 percent for twice the number of years that you went without signing up . For example, if you waited two years to sign up, you will pay the late enrollment penalty for 4 years after signing up.
Is there a penalty for not signing up for Medicare Part B?
If you choose not to sign up for Medicare Part B when you first become eligible, you could face a penalty that will last much longer than the penalty for Part A.
Does Medicare Advantage have penalties?
Medicare Part C (Medicare Advantage) is optional and does not have penalties on its own, but penalties may be included for late enrollment in the parts of Medicare included within your Medicare Advantage plan.
Is Medicare mandatory at 65?
While Medicare isn’t necessarily mandatory, it is automatically offered in some situations, and may take some effort to opt out of.
When did Medicare exempt services start?
Services performed after March 31, 1986, by an employee who was hired by a State or political subdivision employer before April 1, 1986, are exempt from mandatory Medicare coverage if the employee is a member of a public retirement system and meets all of the following requirements: The employee was performing regular and substantial services ...
Is Medicare mandatory for state employees?
State and local government employees hired ( or rehired) after March 31, 1986, are subject to mandatory Medicare coverage. Public employees covered for Social Security under a Section 218 Agreement are already covered for Medicare. Employees whose services are not covered for Social Security but who are required to pay the Medicare-only portion of FICA are referred to as Medicare Qualified Government Employees (MQGE).
