Which of the three types of care in the nursing home will Medicare pay for?
Original Medicare and Medicare Advantage will pay for the cost of skilled nursing, including the custodial care provided in the skilled nursing home for a limited time, provided 1) the care is for recovery from illness or injury – not for a chronic condition and 2) it is preceded by a hospital stay of at least three ...
How many days will Medicare pay 100% of the covered costs of care in a skilled nursing care facility?
20 daysSkilled Nursing Facility (SNF) Care Medicare pays 100% of the first 20 days of a covered SNF stay.
Does Medicare pays most of the costs associated with nursing home care?
If you qualify for short-term coverage in a skilled nursing facility, Medicare pays 100 percent of the cost — meals, nursing care, room, etc. — for the first 20 days. For days 21 through 100, you bear the cost of a daily copay, which was $170.50 in 2019.
What happens when you run out of Medicare days?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
Which type of care is not covered by Medicare?
Medicare and most health insurance plans don't pay for long-term care. Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom.
How much is a nursing home per month?
In 2020, the median yearly cost of nursing home care was $93,075 for a semi-private room and $105,850 for a private room. The median nursing home monthly cost was $7,756 for a semi-private room and $8,821 for a private room. The nursing home monthly cost for a semi-private room increased 3% year-over-year since 2019.Mar 30, 2021
What is considered a skilled nursing facility?
A skilled nursing facility is an in-patient rehabilitation and medical treatment center staffed with trained medical professionals. They provide the medically-necessary services of licensed nurses, physical and occupational therapists, speech pathologists, and audiologists.
What is the average cost of a nursing home by state?
In the United States, the average private room in a nursing home is $8,365 per month or $275 per day. The average cost of a semi-private room is $7,441 per month and $245 per day....Nursing Home Costs by State 2022.StateSemi-Private CarePrivate CareRhode Island$8,821$9,733Washington$8,669$9,718Michigan$8,562$9,125California$8,365$9,81746 more rows
What does Medicare cover for a hospital stay?
Skilled nursing care. Physical, occupational, and/or speech language therapy. Medicare also may cover: A medical social worker. Dietary counseling if indicated. Medical equipment and devices you use during your hospital stay.
What is Medicare Part A?
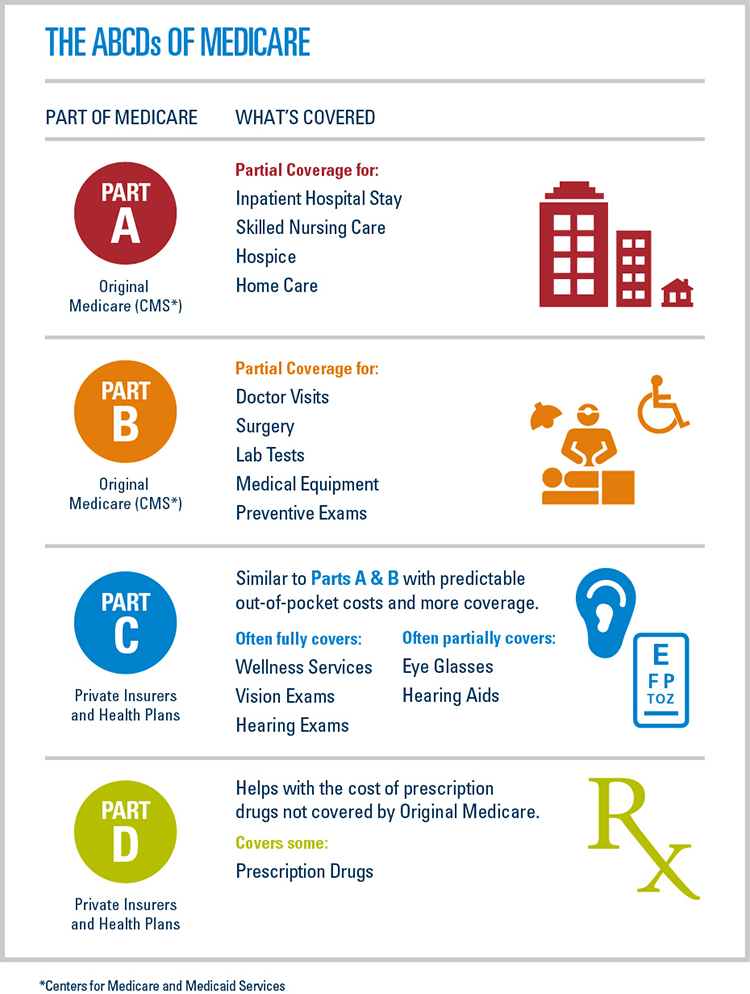
If you have had a qualifying inpatient hospital stay and your doctor orders an additional period of treatment in a skilled nursing facility, Medicare Part A generally covers allowable expenses. Your Part A nursing home benefit usually covers: Physical, occupational, and/or speech language therapy.
What is covered by Part B?
For example, Part B covers your doctor visits and medical therapy visits , and if you need hospital care, Part A benefits apply. If you have a Part D Prescription Drug Plan, the medications you take in the nursing home are usually covered.
Is home care nursing covered by Medicare?
It is usually not covered by Medicare. Home care nursing is generally home health care provided by a credentialed medical professional. It can be short-term while you recover from an illness or injury, or long-term if you have a serious chronic condition or have chosen hospice care.
Does Medicare cover out of pocket expenses?
Medicare Supplement insurance plans may cover your out-of-pocket costs for doctor visits and other medical services covered under Part A and Part B while you are a nursing home resident. You can start comparing Medicare Advantage plans right away – just enter your zip code in the box on this page.
Is long term care covered by Medicare?
As the name suggests, it may last a period of weeks, months, or years. It is usually not covered by Medicare. Home care nursing is generally home health care provided by a credentialed medical professional.
Does Medicare pay for nursing home care?
Medicare does not, however, pay any nursing home costs for long-term care or custodial care. If you need unskilled care for activities of daily living, care for an extended period of time, or care that is not reasonably expected to improve your condition within a limited timeframe, Medicare will not cover it.
What type of insurance covers long term care?
Long-term care insurance. This type of insurance policy can help pay for many types of long-term care, including both skilled and non-skilled care. Long -term care insurance can vary widely. Some policies may cover only nursing home care, while others may include coverage for a range of services, like adult day care, assisted living, ...
How to find out if you have long term care insurance?
If you have long-term care insurance, check your policy or call the insurance company to find out if the care you need is covered. If you're shopping for long-term care insurance, find out which types of long-term care services and facilities the different policies cover.
Do nursing homes accept Medicaid?
Most, but not all, nursing homes accept Medicaid payment. Even if you pay out-of-pocket or with long-term care insurance, you may eventually "spend down" your assets while you’re at the nursing home, so it’s good to know if the nursing home you chose will accept Medicaid. Medicaid programs vary from state to state.
Can federal employees buy long term care insurance?
Federal employees, members of the uniformed services, retirees, their spouses, and other qualified relatives may be able to buy long-term care insurance at discounted group rates. Get more information about long-term care insurance for federal employees.
Does Medicare cover nursing home care?
Medicare generally doesn't cover Long-term care stays in a nursing home. Even if Medicare doesn’t cover your nursing home care, you’ll still need Medicare for hospital care, doctor services, and medical supplies while you’re in the nursing home.
What is an ABN for home health?
The home health agency should give you a notice called the Advance Beneficiary Notice" (ABN) before giving you services and supplies that Medicare doesn't cover. Note. If you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. ...
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
Can you get home health care if you attend daycare?
You can still get home health care if you attend adult day care. Home health services may also include medical supplies for use at home, durable medical equipment, or injectable osteoporosis drugs.
How long does Medicare cover nursing home care?
What parts of nursing home care does Medicare cover? Medicare covers up to 100 days at a skilled nursing facility. Medicare Part A and Part B cover skilled nursing facility stays of up to 100 days for older people who require care from people with medical skills, such as sterile bandage changes.
What is covered by Medicare Advantage?
Some of the specific things covered by Medicare include: A semiprivate room. Meals. Skilled nursing care. Physical and occupational therapy. Medical social services. Medications. Medical supplies and equipment. However, if you have a Medicare Advantage Plan, it’s possible that the plan covers nursing home care.
How many days do you have to be in hospital to qualify for Medicare?
Having days left in your benefit period. Having a qualifying hospital stay of three inpatient days. Your doctor determining that you need daily skilled care.
How much does a nursing home cost?
On average, annual costs for nursing homes fall between $90,000 and $110,000, depending on whether you have a private or semi-private room. This can burn through your personal funds surprisingly quickly. It’s best to pair your personal funds with other financial aid to help you afford nursing home care.
How long does functional mobility insurance last?
Most policies will also require you to pay out of pocket for a predetermined amount of time, usually between 30 and 90 days, before coverage kicks in.
Does Medicare cover dementia care?
Does Medicare cover nursing home care for dementia? Medicare only ever covers the first 100 days in a nursing home, so nursing home coverage is not significantly different for people with dementia. Medicaid can help cover memory care units and nursing home stays beyond 100 days, though. Can older people rely on Medicare to cover nursing home costs? ...
Does Medicare cover nursing home room and board?
It also doesn’t cover room and board for any long-term nursing home stay, including hospice care or the cost of a private room. Lastly, Medicare won’t cover your skilled nursing facility stay if it’s not in an approved facility, so it’s important to know what institutions it has approved in your area.
Does Medicare Cover In
According to the U.S. Department of Health and Human Services, someone turning 65 today has about a 70% chance of needing some type of long-term care in the future.
What Else Should I Be Aware Of
Check if you were admitted as an inpatient. If the hospital classified you as Observation Status, which is an outpatient category, the hospital should have given you a Medicare Outpatient Observation Notice and orally explained the status and how it might affect the cost of your stay.
Do Aetna Medicare Plans Pay For Other Caregiving And Home Health Services
While Medicare Advantage plans are required to meet the above coverage of home health care, Aetna Medicare Advantage plans often go above and beyond to include additional home health care benefits.
How Many Days Will Medicare Pay For Nursing Home Care At A Skilled Nursing Facility
Medicare Part A partially covers costs at an SNF for the first 100 days of each benefit period. A benefit period begins on the day that youre admitted as an inpatient to the SNF or hospital. It ends when you havent received any inpatient care at an SNF or hospital for 60 consecutive days.
Tips On Choosing A Nursing Home
The information contained in this article is for informational purposes only. It should never be used as a substitute for professional medical advice. You should always consult with your medical provider regarding diagnosis or treatment for a health condition.
The Basics Of Paying For Long
Custodial care refers to personal care given to individuals to help them with activities of daily living , which include bathing, dressing, and transferring themselves from seated to standing or in and out of bed. Also known as non-medical care, custodial care can be, and frequently is, provided by persons without professional medical training.
Nursing Homes And Medicare
How Does Medicare Cover Long Term Care, Nursing Home Care, and Skilled Nursing Facility Care?
How long does Medicare cover inpatient hospital stay?
Medicare coverage is provided if all of these conditions are met: You have a qualifying hospital stay of at least three days as an inpatient. This doesn’t include being admitted to the hospital for observation. Your doctor has determined that you need daily skilled care given by skilled nursing or therapy staff.
How many days does Medicare pay for SNF?
Medicare will pay for up to 100 SNF days per rolling benefit period. According to Medicare rules, your benefit period starts the first day you spend as an inpatient at a hospital. That benefit period ends when you haven’t received any inpatient hospital or SNF care for 60 days in a row.
Does Medicare cover nursing home care?
The short answer is, it depends on whether you need long-term care or skilled nursing services. According to Medicare.gov, Medicare Part A (hospital insurance) covers medically necessary care in a skilled nursing facility (SNF) following an acute illness or injury for which you were admitted to a hospital. But if you are in a nursing home only ...
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
Medicare Advantage and Nursing Home Care
In general, Medicare does not cover nursing home care—because it doesn't cover custodial care. According to the official U.S. government website for Medicare, most nursing home care is regarded as custodial care, which is defined as assistance with day-to-day activities like eating, dressing, bathing, and using the bathroom.
Get Started Now
Interested in learning more about Medicare, Medigap, and Medicare Advantage plans? WebMD Connect to Care Advisors may be able to help.
