What is the difference between Medicare and Medicaid?
· To be clear, Medicaid remains available after age 65 and many older adults rely on it — for example, the majority of nursing home residents in the United States have Medicaid coverage in addition to their Medicare coverage. But once you turn 65, eligibility for Medicaid is based on both income and assets.
How to transition to Medicare?
· While Medicare does not provide long-term home and community based benefits, in 2019, some Medicare Advantage plans (Medicare Part C) began to offer such benefits. The Centers for Medicare and Medicaid Services (CMS) oversees both the …
How do you change Medicare coverage?
How to apply for Medicaid. Each state has different rules about eligibility and applying for Medicaid. Call your State Medical Assistance (Medicaid) office for more information and to see if you qualify. You can also call 1-800-MEDICARE (1-800-633-4227) to get the phone number for your state's Medicaid office. TTY users can call 1-877-486-2048.
How to switch your Medicare plan?
When you visit a provider or facility that takes both forms of insurance, Medicare will pay first and Medicaid may cover your Medicare cost-sharing, including coinsurances and copays. Medicaid can provide premium assistance: In many cases, if you have Medicare and Medicaid, you will automatically be enrolled in a Medicare Savings Program (MSP). MSPs pay your …

What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
Can you get Medicaid and Social Security?
SOCIAL SECURITY, MEDICAID AND MEDICARE Many people receive both SSI and Social Security benefits. Medicaid is linked to receipt of SSI benefits in most States. Medicare is linked to entitlement to Social Security benefits. It is possible to get both Medicare and Medicaid.
Who is eligible for Medicaid?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
Is there an age limit for Medicare?
Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How long do you have to be a resident to qualify for medicare?
Persons must be U.S. Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
What is Medicare dual eligible?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program for seniors and disabled persons, Medicaid is a state and federal medical assistance program for financially needy persons of all ages. Both programs offer a variety of benefits, including physician visits and hospitalization, but only Medicaid provides long-term nursing home care. Particularly relevant for the purposes of this article, Medicaid also pays for long-term care and supports in home and community based settings, which may include one’s home, an adult foster care home, or an assisted living residence. That said, in 2019, Medicare Advantage plans (Medicare Part C) began offering some long-term home and community based benefits.
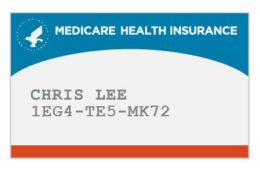
What is Medicare Part A and Part B?
To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
Is Medicare the first payer?
For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid ...
Is Medicare the primary or secondary payer?
For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses.
Is Medicare part of Medicaid?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance).
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare cover medicaid?
If you qualify for a Medicaid program, it may help pay for costs and services that Medicare does not cover.
Is medicaid the primary or secondary insurance?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Does Medicaid offer care coordination?
Medicaid can offer care coordination: Some states require certain Medicaid beneficiaries to enroll in Medicaid private health plans, also known as Medicaid Managed Care (MMC) plans. These plans may offer optional enrollment into a Medicare Advantage Plan designed to better coordinate Medicare and Medicaid benefits.
Do you pay for QMB with Medicare?
If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, coinsurances, and copays. Medicaid can provide prescription drug assistance: Dually eligible individuals are automatically enrolled in the Extra Help program to help with their prescription drug costs.
Your first chance to sign up (Initial Enrollment Period)
Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
Between January 1-March 31 each year (General Enrollment Period)
You can sign up between January 1-March 31 each year. This is called the General Enrollment Period. Your coverage starts July 1. You might pay a monthly late enrollment penalty, if you don’t qualify for a Special Enrollment Period.
Special Situations (Special Enrollment Period)
There are certain situations when you can sign up for Part B (and Premium-Part A) during a Special Enrollment Period without paying a late enrollment penalty. A Special Enrollment Period is only available for a limited time.
Joining a plan
A type of Medicare-approved health plan from a private company that you can choose to cover most of your Part A and Part B benefits instead of Original Medicare. It usually also includes drug coverage (Part D).
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
Can seniors in nursing homes get medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances. It is also common for Medicare beneficiaries who are under 65 and live on Social Security Disability Insurance (SSDI) to receive Medicaid benefits.
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
What percentage of Medicare beneficiaries are dual eligible?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits.
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Does Medicare cover long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care . If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
How long does it take to switch states for medicaid?
After submitting an application, it usually takes between 15 and 90 days to receive a letter of approval.
Can you switch Medicaid coverage?
Because each state has its own Medicaid eligibility requirements, there is no option that allows you to switch Medicaid coverage from one state to another. Therefore, you should reapply for Medicaid in the state where you're planning to live.
When moving to a new state, is it important to transfer your Medicaid benefits?
When relocating to a new state, it's important to transfer your Medicaid benefits to maintain health insurance coverage. Find out what to do to stay covered.
Does Medicaid cover outside of state?
In most cases, Medicaid will not cover services that you receive outside of the state where you live. Although Medicaid is a joint federal and state program, each state administers its own Medicaid program. As a result, eligibility and benefits vary widely by state. Each state also has its own network of providers.
Is Medicaid a federal or state program?
Although Medicaid is a joint federal and state program, each state administers its own Medicaid program. As a result, eligibility and benefits vary widely by state. Each state also has its own network of providers.
Does Medicaid cover out of state medical care?
If you are temporarily out of state, Medicaid will generally only cover services if you encounter a medical emergency that is life-threatening and requires immediate care.
How long does it take to get a letter of approval for medicaid?
After submitting an application, it usually takes between 15 and 90 days to receive a letter of approval. Most states offer retroactive Medicaid coverage, meaning you can receive coverage for medical services prior to the date of your application’s approval.
