Full Answer
How to compare Medicare supplement plans for 2020?
How to Compare Medicare Supplement Plans 1. Plans F and G also offer a high-deductible plan that each have an annual deductible of $2,340 in 2020. Once the... 2. Plan K has an out-of-pocket yearly limit of $5,880 in 2020. After you pay the out-of-pocket yearly limit and yearly... 3. Plan L has an ...
When does Medicare Part D coverage begin and end in 2022?
begins once you reach your Medicare Part D plan’s initial coverage limit ($4,430 in 2022) and ends when you spend a total of $7,050 out-of-pocket in 2022. See: But isn’t the Coverage Gap (Donut Hole) closed?
How do I compare Medicare supplement insurance plans in my area?
A licensed insurance agent can help you compare Medicare Supplement Insurance plans that are available in your area. After you use the comparison chart above, you can ask a licensed agent about the types of Medigap plans that may be offered where you live. Find Medicare Supplement Insurance plans in your area.
How much do you have to pay for Medicare in 2020?
With this option, you must pay for Medicare-covered costs (coinsurance, copayments, and deductibles) up to the deductible amount of $2,340 in 2020 ($2,370 in 2021) before your policy pays anything. (Plans C and F aren't available to people who were newly eligible for Medicare on or after January 1, 2020.)

What is the Medicare premium for 2022?
$170.10The standard Part B premium amount in 2022 is $170.10. Most people pay the standard Part B premium amount. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA).
Are Medicare supplement plans increasing in 2021?
The Medicare Part B premium is $148.50 per month in 2021, an increase of $3.90 since 2020. The Part B deductible also increased by $5 to $203 in 2021. Medicare Advantage premiums are expected to drop by 11% this year, while beneficiaries now have access to more plan choices than in previous years.
When can I choose a new Medicare plan?
From October 15 – December 7 each year, you can join, switch, or drop a plan. Your coverage will begin on January 1 (as long as the plan gets your request by December 7).
Who sells the most Medicare Advantage plans?
UnitedHealthcareStandout feature: UnitedHealthcare offers the largest Medicare Advantage network of all companies, with more than 1 million network care providers. UnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
What are the changes to Medicare in July 2021?
A number of changes will be made to the Medicare Benefits Schedule (MBS) from 1 July 2021, including indexation of most items and changes to general surgery, orthopaedic and cardiac services recommended by the MBS Review Taskforce. The MBS indexation factor for 1 July 2021 is 0.9%.
What is the Medicare premium for 2021?
The Centers for Medicare & Medicaid Services (CMS) has announced that the standard monthly Part B premium will be $148.50 in 2021, an increase of $3.90 from $144.60 in 2020.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Can you change your Medicare plan at any time?
If you enroll during your Initial Enrollment Period, you can also make changes anytime in the first 3 months of your Medicare coverage. “After that, you can switch plans during open enrollment in the Fall or during Medicare Advantage open enrollment, which is at the beginning of each year,” Dworetsky says.
Do you have to change your Medicare plan every year?
In general, once you're enrolled in Medicare, you don't need to take action to renew your coverage every year. This is true whether you are in Original Medicare, a Medicare Advantage plan, or a Medicare prescription drug plan.
What are the top 3 Medicare Advantage plans?
The Best Medicare Advantage Provider by State Local plans can be high-quality and reasonably priced. Blue Cross Blue Shield, Humana and United Healthcare earn the highest rankings among the national carriers in many states.
What percent of seniors choose Medicare Advantage?
[+] More than 28.5 million patients are now enrolled in Medicare Advantage plans, according to new federal data. That's up nearly 9% compared with the same time last year. More than 40% of the more than 63 million people enrolled in Medicare are now in an MA plan.
Are there disadvantages to a Medicare Advantage plan?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
Who sells Medicare Advantage plans?
Medicare Advantage plans are sold by private insurance companies all over the U.S. As a consumer, you can do some research into a company’s history, reputation and ratings before committing to 2019 coverage.
How many stars does Medicare Advantage have?
Each year, the Centers for Medicare & Medicaid Services (CMS) issues star ratings for all Medicare Advantage plans using a system of one to five stars. 1 These plans are evaluated and rated each year, so plan Star Ratings can change each year.
Does Medicare Advantage have a deductible?
Some Medicare Advantage plans may have a higher monthly premium but a lower deductible (or no deductible at all), while other plans may feature $0 premiums but a higher deductible. $0 premium plans may not be available in all locations.
What is the extra Medicare premium called?
Higher income earners may pay higher Medicare Part B and Part D premiums than the standard amount. This extra amount is called the IRMAA, or the Income-Related Monthly Adjusted Amount.
Do Medicare beneficiaries pay a premium?
Most beneficiaries do not pay a premium for their Medicare Part A (hospital insurance) coverage. But those who do pay a Part A premium saw a slight increase in their monthly cost in 2019.
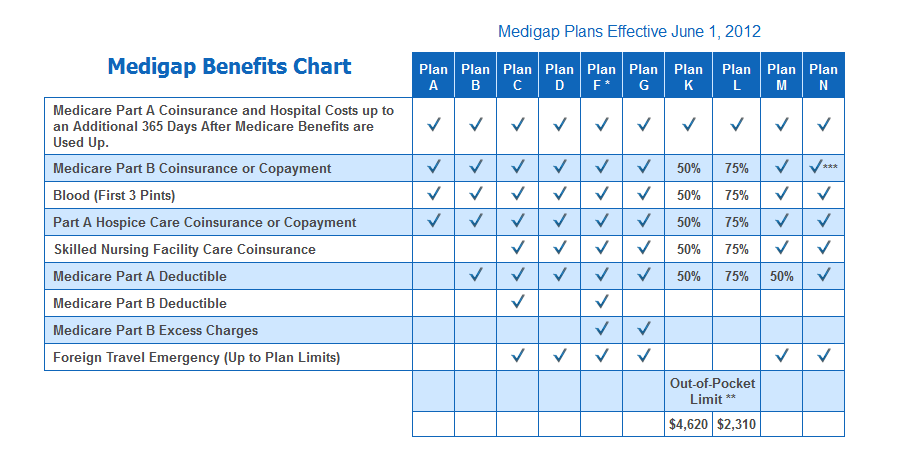
When is Medicare Supplement Chart valid?
This standardized Medicare Supplement chart is valid after June 1, 2010 & updated for 2019. The old plans will no longer be available to purchase after May 31, 2010. Just click on the plan letter to see the specific details about each plan.
When did Medicare standardized?
Medicare standardized the plans in 1990 to limit the consumer’s confusion when comparing coverage offered by different insurance companies.
What does a check mark on a Medicare chart mean?
How to read the chart: If a check mark appears in the column, this means the MediGap policy covers the benefit up to 100% of the Medicare-approved amount. If a dash is in the column the benefit is not covered by the plan.
Is Medicare Supplement interchangeable with MediGap?
The words "Medicare supplement" and MediGap plans are interchangeable and mean exactly ...
Does Medicare Supplement Plan F have a high deductible?
* Medicare Supplement Plan F also has a high deductible option. We don't recommend the high deductible plan F in most cases.
Who is Medicare.net?
Medicare.net is powered by Health Network Group, LLC, which is related to Health Compare Insurance Services, Inc., who is a licensed, authorized agent of: Anthem Blue Cross of California, Anthem Blue Cross of Colorado, Anthem Blue Cross of Connecticut, Anthem Blue Cross of Georgia, Anthem Blue Cross of Indiana, Anthem Blue Cross of Kentucky, Anthem Blue Cross of Maine, Anthem Blue Cross of Missouri, Anthem Blue Cross of New Hampshire, Anthem Blue Cross of Nevada, Anthem Blue Cross of New York, Anthem Blue Cross of Ohio, Anthem Blue Cross of Texas, Anthem Blue Cross of Virginia, Anthem Blue Cross of Wisconsin, Blue Cross Blue Shield of Illinois, Blue Cross Blue Shield of Montana, Blue Cross Blue Shield of New Mexico, Blue Cross Blue Shield of Oklahoma, Capital Blue Cross of Pennsylvania, Highmark of West Virginia, Premera in Washington, Premera in Alaska, and Vibra in Pennsylvania.
How much is United Health Care Sync?
The monthly premium for the UnitedHealthcare Sync PPO plan is $54. Primary care visits have a $15 copay while specialists have a $50 copay. Routine physicals are free, and there’s no annual deductible for medical services. The maximum you’ll pay for in-network services for the year is $5,900. Inpatient hospital stays require a $400 copay per day for days 1 through 4, but there’s no copay for days 5 through 90. Skilled nursing facility costs are also covered.
How much does Aetna pay for medical?
Under the Aetna Medicare Choice Plan, if you are between the ages of 65 and 69 in fair health, the monthly premium is $73, and you can expect to pay approximately $3,738 per year for medical costs, including premiums. There is no deductible if you remain in the network, but if you go outside the network you’ll have to meet a $750 deductible before benefits start. There’s an annual cap on your out-of-pocket costs with this plan of $6,700 (for in-network services). In-network primary care physician copays are $5 and 40 percent outside the network. Specialists are $40 in-network and 40 percent outside the network. Inpatient hospital stays cost $220 per day for the first four days. After that, you won’t have to pay a copay for inpatient stays.
What is Humana Gold Choice?
Humana Gold Choice PFFS covers many of the same benefits as all Humana Medicare Advantage plans in 2019, including everything that original Medicare covers along with added features and services. With this plan, the monthly premium is about $94, and there’s a $200 medical deductible whether you get care from an in-network or out-of-network provider (for services not covered under original Medicare). Primary doctors require a $20 copay while specialists will cost $50 per visit. This plan and the other two outlined above require a $25 copay for visits to an urgent care center and a $90 copay for emergency room visits. There’s also an out-of-pocket cap in place for covered services of $6,700.
How much is BlueMedicare Choice HMO?
BlueMedicare Choice HMO has a $42 monthly premium and primary care visits have $10 copay. Specialists have a $45 copay while inpatient hospital facility services are $290 copay per day for days 1 through 5. Urgent care facilities are $50 copay and emergency room visits have a copay of $90, but this may be waived if you are admitted.
Is there a premium for BlueMedicare?
There is no premium for BlueMedicare Preferred POS. Primary care office visits have a $0 copay while specialists have a $25 copay. Days 1 through 5 of a hospital stay require a copay of $120 per day, and urgent care facilities have a $25 copay. Emergency room services, both in and out-of-network, are $85 but the fee may be waived if you get admitted.
Is Humana Medicare Advantage?
Humana offers a wide range of insurance products, one of their most prominent being Medicare Advantage. Founded in Kentucky in 1961, the company consistently ranks on lists of top employers in the country, and its commitment to corporate social responsibility sets it apart from industry leaders. In Meomonee Falls, Wisconsin, there are nine Medicare Advantage plans available. We’ve highlighted a few in this section.
How much is Medicare deductible for 2020?
With this option, you must pay for Medicare-covered costs (coinsurance, copayments, and deductibles) up to the deductible amount of $2,340 in 2020 ($2,370 in 2021) before your policy pays anything. (Plans C and F aren't available to people who were newly eligible for Medicare on or after January 1, 2020.)
What is coinsurance in Medicare?
Coinsurance is usually a percentage (for example, 20%). The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. (unless the Medigap policy also pays the deductible).
What states have Medigap policies?
In Massachusetts, Minnesota, and Wisconsin, Medigap policies are standardized in a different way. Each insurance company decides which Medigap policies it wants to sell, although state laws might affect which ones they offer. Insurance companies that sell Medigap policies:
What is covered benefits?
benefits. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents. but some offer additional benefits, so you can choose which one meets your needs.
Where do you live in Medigap?
You live in Massachusetts, Minnesota, or Wisconsin. If you live in one of these 3 states, Medigap policies are standardized in a different way. You live in Massachusetts. You live in Minnesota. You live in Wisconsin.
Do insurance companies have to offer every Medigap plan?
Insurance companies that sell Medigap policies: Don't have to offer every Medigap plan. Must offer Medigap Plan A if they offer any Medigap policy. Must also offer Plan C or Plan F if they offer any plan.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
