
When does Medicaid end for a child?
Your child’s Medicaid coverage will end once they turn 18 years of age. At this point, they will legally be an adult and will have to apply for regular Medicaid or some other type of health coverage. They have a disability.
Can children be on Medicaid?
The Medicaid program provides coverage to 27 million children under age 18 in the United States. According to the U.S. Surgeon General, while 11 percent of youth have been diagnosed with a mental illness, two-thirds of youth who have a condition are not identified and do not receive mental health service.
Who is eligible for Medicaid?
— The Department of Human Services (DHS) must routinely check whether recipients of public assistance are still eligible for the Supplemental Nutrition Assistance Program (SNAP) or Medicaid. — Applicants for SNAP would be required to cooperate with child support in order to qualify for the program.
What age does Medicaid stop?
This policy brief uses the most recent available data to examine the patterns of health coverage for young adults after they turn 19 and typically are no longer eligible for Medicaid or the Children’s Health Insurance Program (CHIP).
Are children included in Medicare?
Summary: Medicare is individual insurance, not family insurance, and coverage usually does not include spouses and children. Unlike other types of insurance, Medicare is not offered to your family or dependents once you enroll. To get Medicare, each person must qualify on their own.
What age do you start Medicare?
65 or olderMedicare is health insurance for people 65 or older. You're first eligible to sign up for Medicare 3 months before you turn 65. You may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease (ESRD), or ALS (also called Lou Gehrig's disease).
What is the difference between the Medicaid and Medicare?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
Who qualifies for Medicaid?
To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, 177.87 KB).
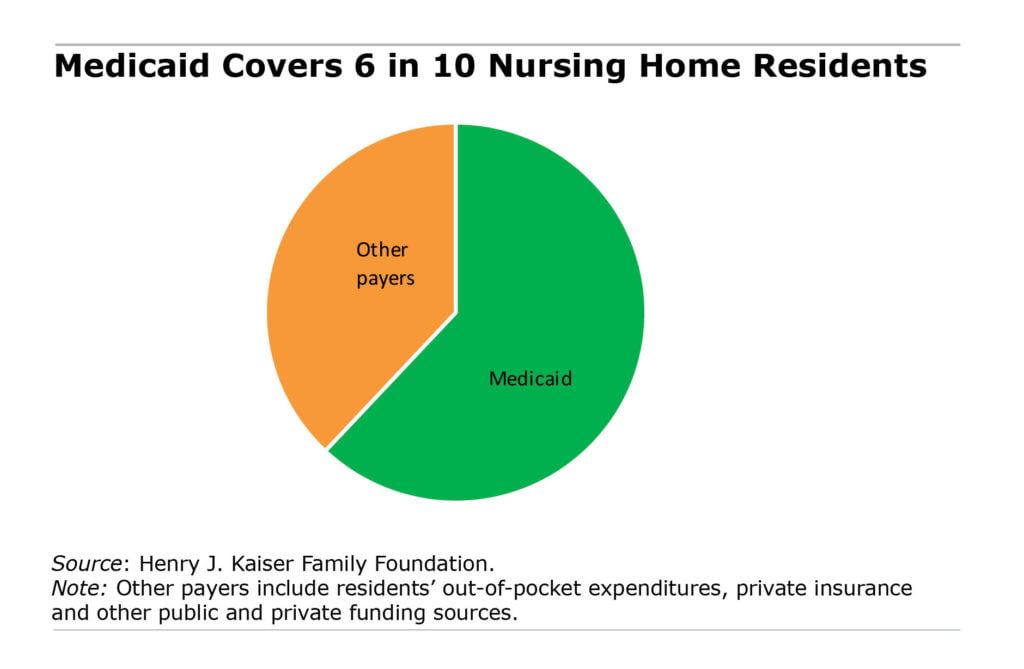
Who is covered by Medicaid?
In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. In some states the program covers all low-income adults below a certain income level.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What is not covered by Medicaid?
Medicaid is not required to provide coverage for private nursing or for caregiving services provided by a household member. Things like bandages, adult diapers and other disposables are also not usually covered, and neither is cosmetic surgery or other elective procedures.
Can you have Medicare and Medicaid at the same time?
Yes. A person can be eligible for both Medicaid and Medicare and receive benefits from both programs at the same time.