Medicare coverage of chiropractic services may require the use of specific modifier codes. The AT Modifier is used to indicate that the covered services billed are for active corrective treatment and the provider’s documentation supports medical necessity and Medicare coverage guidelines. The GA, GX, GY and GZ modifiers can also be used to indicate services that are expected to be denied because of lack of medical necessity or statutory exclusion, and those that do not meet the definition ...
Can chiropractor use GP modifier?
Secondly, can a chiropractor use a GP modifier? According to CMS, a GP modifier means services are delivered under an outpatient physical therapy plan of care. For Medicare claims, chiropractors must include modifier GP on all physical medicine codes to receive a proper denial of patient responsibility so a secondary payer may make payment.
What are the Medicare guidelines for chiropractic?
- § 30.5 Chiropractor’s Services
- § 40.4 Definition of Physician /Practitioner.
- § 220 Coverage of Outpatient Rehabilitation Therapy Services (Physical Therapy, Occupational Therapy, and Speech-Language Pathology Services) Under Medical Insurance
- §240 Chiropractic Services - General
- §240.1.1 Manual Manipulation
How to Bill chiropractic claims?
You'll learn:
- Basics of billing for a chiropractic practice
- The most common code modifiers
- How to file claims with Medicare and private insurance
- Specifics for submitting workers' compensation and auto accident claims
- How to handle prior authorizations and benefits verification
What is means of modifier in medical billing?
What is Modifiers in Medical Billing and Coding? A CPT Modifier is a two-position alpha and alpha-numeric code used to identify certain situations that require the basic value of a procedure to be either enhanced or diminished. A modifier provides the means by which a service or procedure that has been performed can be altered without changing the procedures code. Modifying circumstances include. CPT Modifiers are an important part of the managed care system or medical billing.

What modifiers are used for chiropractic billing?
Modifiers in Chiropractic Medical Billing:Modifier 25. Modifier 25 is utilized to show that this is an important, independently recognizable evaluation and management (E/M) service by the same physician on the same day. ... GA Modifier. ... GY Modifier. ... Modifier 59. ... X-set Modifiers. ... The Active Treatment (AT) Modifier.
Does Medicare require modifier at for chiropractic?
For Medicare purposes, a doctor of chiropractic must place an AT modifier on a claim when providing active/corrective treatment to treat acute or chronic subluxation. However, the presence of the AT modifier may not in all instances indicate that the service is reasonable and necessary.
How do I bill chiropractic to Medicare?
Diagnosis Code Description Medicare Covered Chiropractic Services If the CPT code is 98940, 98941, or 98942 and is billed with one of the following primary diagnosis codes and with modifier AT, then the chiropractic service is covered.
What is a 21 modifier used for?
Use modifier -21, “Prolonged Evaluation and Management Services,” when an E/M service takes more time than is usually required for the highest level of service within a given E/M category.
What is a 59 modifier chiropractic?
Modifier 59 allows the claim to pass Medicare bundling edits, which would lead to additional reimbursement for the physician. Chiropractic manipulative treatment codes — 98940, 98941, and 98942 — comprise three procedures, that is, pre-assessment (history), manipulation, and post-assessment, bundled together.
What is modifier at in chiropractor?
The Active Treatment (AT) modifier was developed to clearly define the difference between active treatment and maintenance treatment. Medicare pays only for active/corrective treatment to correct acute or chronic subluxation. Medicare does not pay for maintenance therapy.
Does 98943 need a modifier?
Simply code it as 98943, no modifiers necessary. Make sure that you have an appropriate diagnosis code that reflects the extremity problem.
Does 97010 need a modifier?
This policy change requires that claims with physical medicine services 97010-97799 will require modifier GP. The modifier is required for dates of service after April 1, 2021.
How do you code chiropractic services?
The most commonly billed chiropractic CPT codes are CPT Code 98940 Chiropractic manipulative treatment (CMT); Spinal, 1-2 regions, CPT Code 98941 Chiropractic manipulative treatment (CMT); Spinal, 3-4 regions, and CPT Code 98942 Chiropractic manipulative treatment (CMT); Spinal, 5 regions.
What is 23 modifier used for?
Modifier 23 is used only with general or monitored anesthesia codes (CPT codes 00100- 01999). Modifier 23 is added after the primary anesthesia modifier which identifies whether the service was personally performed, medically directed or medically supervised (Modifiers AA, AD, QK, QS, QX, QY or QZ).
What is the 32 modifier used for?
When to use Modifier 32. Modifier -32 indicates a service that is required by a third-party entity, Worker's Compensation, or some other official body. Modifier 32 is no used to report a second opinion request by a patient, a family member or another physician. This modifier is used only when a service is mandated.
What is modifier 29 used for?
CPT Modifier 29 (DELETED) CPT modifier 29 was used for global procedures. These are services where one provider is responsible for both the professional and a technical component. Note: Modifier 29 has been deleted. If a provider is billing for a global service, no modifier is necessary.
Can You Tell Me A Little More About Your Company?
We are a San Francisco based company that provides an end-to-end platform for wellness providers like chiropractors. We are bringing a Silicon Vall...
Can You Please Explain The Differences Between Your Monthly Plans?
We have 3 different plans to help with your chiropractic practice management. All 3 plans provide basic Chiropractic EHR features including: Online...
Do I Have To Sign A Contract?
Yes, our pricing model is based on an annual contract. Let us explain why. Our onboarding process focuses on a hassle free migration from your exis...
What Separates zHealthEHR From Other Chiropractic Software Vendors?
Great question! Below are some of our key features that will make you chose zHealthEHR over other vendors. A 100% cloud-based Chiropractic EHR Soft...
Why Do You Have 3 Different Plans For Chiropractic Practice Management Software? Isn't it confusing?
We at zHealthEHR do not nickel and dime our customers. We grow along with your practice and want to provide flexibility by offering multiple choice...
Do You Charge More For Additional Users?
Any number of your front desk staff, office managers, or billing personnel can access a single subscription of zHealthEHR. We only charge per chiro...
Do You Provide Managed Billing Services?
Yes! We do provide Managed Billing Services. This includes the following: Demographic entry Charge entry, Claim Submission, Filing Coding Payment p...
How Much Does zHealthEHR Managed Billing Services Cost?
zHealthEHR charges 5% of the total (gross) amount collected from ALL insurance companies and ALL patients (excluding co-pay) as a result of the bil...
Can I Switch Plans In The Middle Of A Contract If I Decide To Upgrade Later?
We at zHealthEHR are always on your team. You can upgrade your plan at any time to utilize additional features that boost your practice.
Do You Charge Extra For Software Updates And Data Storage?
Software updates and data storage are free and secure. These items are included in your subscription plan. Updates are installed automatically with...
What is a modifier in chiropractic billing?
Modifiers are a vital part of billing for health care services including Chiropractic and are most usually used to recognize specific CPT codes, to keep them from being packaged into another service and charged on the same day.
What is separate practitioner XP?
XP Separate Practitioner: A Service That Is Distinct Because It Was Performed By A Different Practitioner
Is chiropractic adjustment covered by Medicare?
Added to all service does except the CMT for Medicare claims as all services except the Chiropractic Adjustment are not covered under the Medicare Program when rendered by a chiropractor.
What does modifier mean in a treatment?
Anytime you build any type of treatment, you must indicate that the exam is above and beyond. This modifier indicates that it’s a separately identifiable service. In other words, the treatment itself includes a little bit of exam. By example, on the first visit with someone you’re going to do a very detailed exam.
What is a modifier in a claim?
Modifiers are referred to as level one modifiers that are used to supplement information about a claim. By example, you’re all familiar with like using modifier 25. It’s there to tell them that the exam is separate. So really modifiers, just do additional things to allow us to know something about the code.
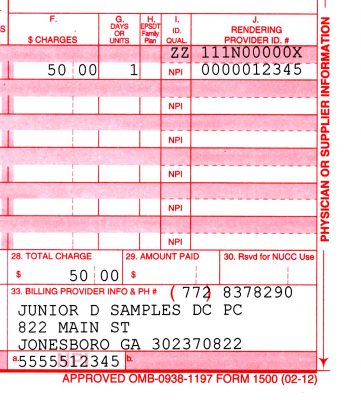
What does a modifier do on a 1500 form?
It’s there to tell them that the exam is separate. So really modifiers, just do additional things to allow us to know something about the code. Remember there always two characters. Sometimes they are numbers. Sometimes they are letters now. So modifiers don’t typically alter the payment. It doesn’t increase the fee. Doesn’t decrease it. But what a modifier does is to make sure the claim does get paid. So the modifiers go right in this section of the 1500 form notice there’s four spaces. Now some of you may be going back to when this code or when this form updated many years ago, why four spaces while I think it was an in anticipation of what we’re seeing now, which is this update to the use of different types of modifiers. So what I want you to see here is that there are four spaces for modifiers, and there could be instances where you may use all four, not typical, but could, I’d say it’s not uncommon though, for a chiropractor to use three, but what’s the most common chiropractic modifier.
Is massage a modifier?
However, there’s a problem with these because there’s a modifier necessary. If without that modifier, you will not be paid.
Do modifiers increase or decrease the fee?
So modifiers don’t typically alter the payment. It doesn’t increase the fee. Doesn’t decrease it. But what a modifier does is to make sure the claim does get paid. So the modifiers go right in this section of the 1500 form notice there’s four spaces.
Does Medicare require a modifier for a gyn?
Once it’s maintenance care, if you choose to, you can charge your regular rate. So Medicare requires an 18 modifier, manipulation, a GYN on every other service cause it’s excluded. But if it’s physical medicine, a GP, and if it is maintenance care, then G Y we are something unique.
Is a GP required for physical therapy?
Well GP, because as a doctor of chiropractic, you’re really doing physical medicine as an adjunct. So hence why we put a GP when it comes to physical medicine codes that G geo would be for an occupational therapist in G and first purpose. So therefore it would be, you know, where is this required? Well, it’s required on all physical medicine and rehabilitation services. So that means any of the physical therapy codes, which would be codes nine seven zero one zero through nine seven, nine, nine. And this included from last year, April of 2020 United healthcare and any affiliates. So that includes OptumHealth UMR in any of those. But in addition recently, it’s also required. Of course, if you’re billing VA claims also beginning this year, it’s required on blue cross blue shield plans of Michigan blue cross of California. Now be careful if you’re in California, not blue shield, but blue cross other States with blue cross blue shield include Indiana, Kentucky, Missouri, New Jersey, New York.
Why do chiropractors need to coding?
Besides tracking the patient’s medical history, coding helps in receiving insurance payouts on time. It is challenging to determine the medical codes for chiropractors, and it takes a lot of time. So one can also consider outsourcing the same, so as to be relieved of the lengthy process.
What is CPT in chiropractic?
What is CPT? The American Medical Association is responsible for mainly publishing and maintaining the Chiropractic CPT Codes and specifications. These codes are considered some of the essential principles for chiropractors, and they have to become familiar with the same.
What is a CPT code?
CPT codes make an integral part of the entire chiropractic billing process. Chiropractic billing codes tell the insurance company what procedures the chiropractor is performing and would like to be reimbursed for. Insurance companies use CPT codes to track health data and measure specific medical procedures’ prevalence and value.
How many characters are in CPT codes?
All the CPT codes tend to feature five alpha-numeric characters, which describe evaluations, diagnostic tests, and medical procedures. All of them are performed either by a doctor or a chiropractor on a patient. The codes tend to contain tens of thousands of medical procedures as they are huge.
Is chiropractic practice difficult?
It is pretty challenging to run chiropractic practice as it tends to take relatively longer to process the treatments, and in the wake of the same, the other essential tasks go unnoticed. Effective chiropractic medical billing and coding practices share several elements in common. This includes a properly trained staff, proper coding and documentation, deft practice management, and a healthy accounts receivable, taking care of ICD10/CPT Coding services amongst a lot more.
Can chiropractic be reimbursed?
There is nothing surprising to know that chiropractic billing can be challenging, but the reimbursements can happen successfully with perfect CPT codes.
When do chiropractors have to use the AT modifier?
For Medicare purposes, a chiropractor must place an AT modifier on a claim when providing active/corrective treatment to treat acute or chronic subluxation. However, the presence of the AT modifier may not in all instances indicate that the service is reasonable and necessary.
What is a modifier in Medicare?
A modifier comprises two alpha, numeric, or alphanumeric characters reported with a HCPCS code, when appropriate. Modifiers are designed to give Medicare and commercial payers additional information needed to process a claim. This includes HCPCS Level I (Physicians’ Current Procedural Terminology [CPT®]) and HCPCS Level II codes. The reporting physician appends a modifier to indicate special circumstances that affect the service provided without affecting the service or procedure description itself. When applicable, the appropriate two-character modifier code should be used to identify the modifying circumstance. The modifier should be placed after the usual procedure code number.
What is an ABN for a chiropractor?
You should consider providing the Advance Beneficiary Notice of Noncoverage (ABN) to the beneficiary. Chiropractors who give beneficiaries an ABN will place the modifier GA (or in rare instances modifier GZ) on the claim. The decision to deliver an ABN must be based on a genuine reason to expect that Medicare will not pay for a particular service on a specific occasion for that beneficiary due to lack of medical necessity for that service. The beneficiary can then make a reasonable and informed decision about receiving and paying for the service. If the beneficiary decides to receive the service, you must submit a claim to Medicare even though you expect that Medicare will deny the claim and that the beneficiary will pay.
What is AT modifier?
The Active Treatment (AT) modifier was developed to clearly define the difference between active treatment and maintenance treatment. Medicare pays only for active/corrective treatment to correct acute or chronic subluxation. Medicare does not pay for maintenance therapy. Claims should include a primary diagnosis of subluxation ...
What is the purpose of modifier 24?
Modifier 24 is added to the selected E/M service code to identify the E/M service rendered by the same provider as unconnected and distinct from other services in the patient’s postoperative period.
When does CPT 98940 need to be included?
The policy requires the following: 1. Every chiropractic claim for CPT 98940/98941/98942, with a date of service on or after October. 1, 2004, should include the AT modifier if active/corrective treatment is being performed; and. 2. The AT modifier should not be used if maintenance therapy is being performed.
When do you need to use the AT modifier?
You must place the AT modifier on a claim when providing active/corrective treatment to treat acute or chronic subluxation. However, the presence of the AT modifier may not in all instances indicate that the service is reasonable and necessary.