What is the Medicare reimbursement form?
The Medicare reimbursement form, also known as the “Patient’s Request for Medical Payment,” is available in both English and Spanish on the Medicare website. To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request.
How many terms are in the medical billing and reimbursement system?
Medical Terms HCC PTA 99 terms sarahg1206 Sets with similar terms Medical Billing and Reimbursement Systems 46 terms Michelle_Smith Billing and Coding Definitions 133 terms vnsgorham Test 3 95 terms
How do I request reimbursement from my doctor?
If you want Medicare to pay for your care, you’ll need to send a form to request reimbursement. These doctors accept Medicare patients, but they haven’t agreed to Medicare’s rates. They may choose to accept Medicare rates in your case, or they may decide to bill you up to 15% more than the Medicare rate.
How does Medicare work for Medicare recipients?
For Medicare recipients, however, the system may work a little bit differently. When someone who receives Medicare benefits visits a physician’s office, they provide their Medicare information, and instead of making a payment, the bill gets sent to Medicare for reimbursement.
What reimbursement method does Medicare use?
A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).
What does Medicare reimbursement depend on?
Medicare reimbursement rates depend on the number of individual services provided to the patient in one day. Similar to its hospital inpatient counterpart, the OPPS also provides some hospitals with add-on payments.
What does reimbursement mean in medical terms?
Learn about our editorial process. Healthcare reimbursement describes the payment that your hospital, healthcare provider, diagnostic facility, or other healthcare providers receive for giving you a medical service. Often, your health insurer or a government payer covers the cost of all or part of your healthcare.
How does Medicare reimburse healthcare organizations?
Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement. Providers have an agreement with Medicare to accept the Medicare-approved payment amount for their services.
What is reimbursement payment?
Reimbursement is compensation paid by an organization for out-of-pocket expenses incurred or overpayment made by an employee, customer, or another party. Reimbursement of business expenses, insurance costs, and overpaid taxes are common examples.
How are reimbursement rates determined?
Payers assess quality based on patient outcomes as well as a provider's ability to contain costs. Providers earn more healthcare reimbursement when they're able to provide high-quality, low-cost care as compared with peers and their own benchmark data.
What is the abbreviation for reimbursement?
reimbSummary: Reimbursement Abbreviation There is one common abbreviation of reimbursement: reimb.
What are reimbursement codes?
ReimbursementCodes is a software-as-a-service application designed to minimize the reimbursement risk and delayed processing, for both provider and payor groups.
What are the four main methods of reimbursement?
Here are the five most common methods in which hospitals are reimbursed:Discount from Billed Charges. ... Fee-for-Service. ... Value-Based Reimbursement. ... Bundled Payments. ... Shared Savings.
What are reimbursement models?
Healthcare reimbursement models are billing systems by which healthcare organizations get paid for the services they provide to patients, whether by insurance payers or patients themselves.
Why do doctors accept Medicare?
The reason so many doctors accept Medicare patients, even with the lower reimbursement rate, is that they are able to expand their patient base and serve more people.
What happens when someone receives Medicare benefits?
When someone who receives Medicare benefits visits a physician’s office, they provide their Medicare information , and instead of making a payment, the bill gets sent to Medicare for reimbursement.
Do you have to pay Medicare bill after an appointment?
For some patients, this means paying the full amount of the bill when checking out after an appointment, but for others , it may mean providing private insurance information and making a co-insurance or co-payment amount for the services provided. For Medicare recipients, however, the system may work a little bit differently.
Can a patient receive treatment for things not covered by Medicare?
A patient may be able to receive treatment for things not covered in these guidelines by petitioning for a waiver. This process allows Medicare to individually review a recipient’s case to determine whether an oversight has occurred or whether special circumstances allow for an exception in coverage limits.
What is covered entity?
a covered entity means an organization that routinely handles protected health information.Individuals , organizations and agencies that meet the definition of a covered entity must comply with the HIPAA rules to protect health information. EOB. EOB is Explanation of Benefits. Episode of Care reimbursement.
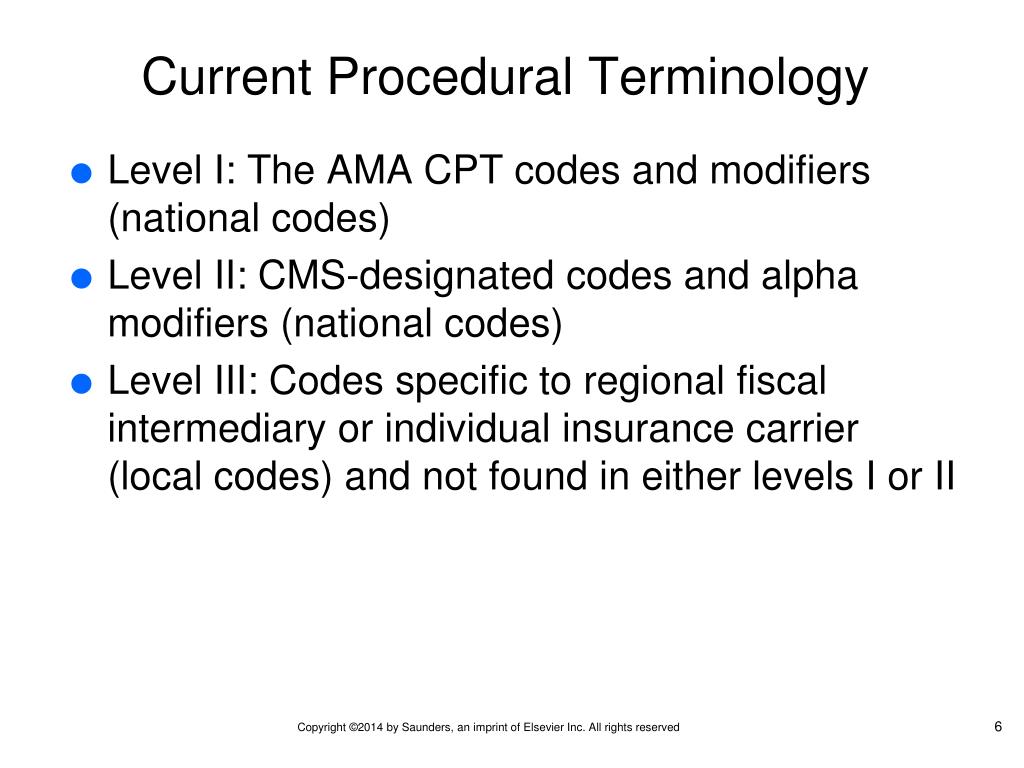
Is CPT assigned inpatient?
CPT® or HCPCS codes are not assigned in the inpatient setting. Home Health Prospective Payment System - a prospective payment system because reimbursement rates are set in advance for home healthcare. Reimbursement rates are paid for 60-day blocks of time.
