
Who would not be covered under Medicare?
Some of the items and services Medicare doesn't cover include:Long-Term Care. ... Most dental care.Eye exams related to prescribing glasses.Dentures.Cosmetic surgery.Acupuncture.Hearing aids and exams for fitting them.Routine foot care.
Does everyone qualify for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Why can you be denied Medicare?
Medicare can deny coverage if a person has exhausted their benefits or if they do not cover the item or service. When Medicare denies coverage, they will send a denial letter. A person can appeal the decision, and the denial letter usually includes details on how to file an appeal.Aug 20, 2020
Who is denied Medicare?
Medicare may issue denial letters for various reasons. Example of these reasons include: You received services that your plan doesn't consider medically necessary. You have a Medicare Advantage (Part C) plan, and you went outside the provider network to receive care.May 18, 2020
Can you be denied Medicare?
In all but four states, insurance companies can deny private Medigap insurance policies to seniors after their initial enrollment in Medicare because of a pre-existing medical condition, such as diabetes or heart disease, except under limited, qualifying circumstances, a Kaiser Family Foundation analysis finds.Jul 11, 2018
Can my wife get Medicare if she never worked?
If you don't have enough work quarters to qualify for premium-free Part A through your own work history, you may be able to qualify through your spouse. Note that you'll both have to separately enroll in Medicare, but neither of you would have to pay a monthly premium for Part A.
What is IDN letter?
Medicare health plans are required to issue the Notice of Denial of Medical Coverage (or Payment), also known as the Integrated Denial Notice (IDN), upon denial, in whole or in part, of an enrollee's request for coverage and upon discontinuation or reduction of a previously authorized course of treatment.Dec 1, 2021
What do I do if Medicare won't pay?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
Does AARP cover pre-existing conditions?
A: Coverage includes doctor visits, hospitalizations and prescription drugs. Enrollees will get better benefits when they use in-network providers. There are no waiting periods, and pre-existing conditions are covered.
What is Medicare denial Code N211?
Reason Code 29 | Remark Code N211CodeDescriptionReason Code: 29The time limit for filing has expired.Remark Code: N211You may not appeal this decision.Jan 14, 2021
What age do you have to be to get Medicare?
You must also meet at least one of the following criteria for Medicare eligibility: Be age 65 or older and eligible for Social Security: You may be automatically enrolled in Medicare Part A (hospital insurance) when you reach age 65 and become eligible for Social Security. But, if you’re not receiving retirement benefits from Social Security or ...
What happens if you don't sign up for Medicare Part B?
Be aware that if you don’t sign up for Medicare Part B when you first become eligible, you may have to pay a 10% penalty (added to your monthly premium) for each full 12-month period you could have had it but didn’t sign up (some exceptions apply).
How long does Medicare Advantage last?
The Medicare Advantage plan (Part C) Initial Coverage Election Period is generally the same as the Initial Enrollment Period for Medicare Part A and Part B (the seven-month period that starts 3 months before the month you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65).
What is Medicare Part C?
Medicare Part C (also called Medicare Advantage ) is an alternative way to get your Medicare Part A and Part B benefits. Medicare Advantage plans are available through private insurers. To be eligible for Medicare Part C, you must already be enrolled in Medicare Part A and Part B, and you must reside within the service area ...
How long do you have to be disabled to get a disability?
Be permanently disabled and receive disability benefits for at least two years: You automatically get Part A and Part B after you get disability benefits from Social Security for 24 months or certain disability benefits from the Railroad Retirement Board (RRB) for 24 months. Have end-stage renal disease (ESRD) (permanent kidney failure ...
How much is the Part B premium for 2021?
In addition, you must also pay the Part B premium each month. The standard premium is $148.50 in 2021. Also, keep in mind that individuals with a higher income may have to pay more for their Part B premium.
Does Medicare Part D cover prescription drugs?
Medicare Part D covers prescription drugs and , like Medicare Part C, is available through private insurers that are approved by Medicare. To be eligible to enroll in a Medicare prescription drug plan (PDP), you must have Medicare Part A and/or Part B and you must live in the service area for the prescription drug plan in which you want to enroll.
How old do you have to be to get Medicare?
citizen or have been a legal resident for at least five years, you can get full Medicare benefits at age 65 or older. You just have to buy into them by: Paying premiums for Part A, the hospital insurance.
How long do you have to live to qualify for Medicare?
You qualify for full Medicare benefits if: You are a U.S. citizen or a permanent legal resident who has lived in the United States for at least five years and. You are receiving Social Security or railroad retirement benefits or have worked long enough to be eligible for those benefits but are not yet collecting them.
How much will Medicare premiums be in 2021?
If you have 30 to 39 credits, you pay less — $259 a month in 2021. If you continue working until you gain 40 credits, you will no longer pay these premiums. Paying the same monthly premiums for Part B, which covers doctor visits and other outpatient services, as other enrollees pay.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security disability benefits for at least 24 months (that need not be consecutive); or. You receive a disability pension from the Railroad Retirement Board and meet certain conditions; or.
What is Lou Gehrig's disease?
You have Lou Gehrig’s disease, also known as amyotrophic lateral sclerosis (ALS), which qualifies you immediately; or. You have permanent kidney failure requiring regular dialysis or a kidney transplant — and you or your spouse has paid Social Security taxes for a specified period, depending on your age.
How old do you have to be to get medicare?
Who is eligible for Medicare? Medicare coverage starts at age 65 for everyone who is either a U.S. citizen, or has been a permanent legal resident for at least five years.
What are the requirements for Medicare?
There are also a few conditions that will qualify you for Medicare coverage prior to age 65, including: 1 You are permanently disabled and have received disability benefits for at least two years. 2 You have End-Stage Renal Disease requiring dialysis, or have had a kidney transplant. 3 You have ALS -- which is more commonly known as Lou Gehrig's disease.
What is Medicare insurance?
Medicare is the federal health-insurance program that provides coverage for millions of retired and disabled Americans. While the government has made efforts to make it easy for participants to sign up for Medicare benefits, there are a handful of eligibility hurdles that potential enrollees need to be aware of. Who is eligible for Medicare?
How long do you have to be disabled to receive disability?
You are permanently disabled and have received disability benefits for at least two years. You have End-Stage Renal Disease requiring dialysis, or have had a kidney transplant. You have ALS -- which is more commonly known as Lou Gehrig's disease.
Can I apply for Medicare if I have end stage renal disease?
You have End-Stage Renal Disease and qualify for Medicare. You live in Puerto Rico and are automatically enrolled in Part A, but want to add Part B coverage, too. Thankfully, its easy to apply online for Medicare, so your benefits will start on time.
How long do you have to be on Part A and Part B?
If you are under 65 and have a disability, you are also automatically enrolled in Part A and Part B if you receive Social Security benefits, or certain disability benefits from the RRB for 24 months. If you have ALS.
How do I contact Social Security?
You can also visit a local Social Security office if you need help, or can call 1-800-772-1213 if you prefer to use the phone (railroad workers should call the RRB at 877-772-5772). If you meet the eligibility criteria and have not yet enrolled, it's generally smart not to wait.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
What is MEC in Medicare?
Medicare and Minimum Essential Coverage (MEC) Medicare Part A counts as minimum essential coverage and satisfies the law that requires people to have health coverage. For additional information about minimum essential coverage (MEC) for people with Medicare, go to our Medicare & Marketplace page.
What age do you have to be to get a Social Security card?
Understanding the Rules for People Age 65 or Older. To be eligible for premium-free Part A on the basis of age: A person must be age 65 or older; and. Be eligible for monthly Social Security or Railroad Retirement Board (RRB) cash benefits.
How long does Part A coverage last?
If the application is filed more than 6 months after turning age 65, Part A coverage will be retroactive for 6 months. NOTE: For an individual whose 65th birthday is on the first day of the month, Part A coverage begins on the first day of the month preceding their birth month.
When do you get Part A?
An individual who is receiving monthly Social Security or RRB benefits at least 4 months prior to turning age 65 does not need to file a separate application to become entitled to premium-free Part A. In this case, the individual will get Part A automatically at age 65.
What is the income related monthly adjustment amount?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount.
How long do you have to wait to get Medicare Supplement?
Keep in mind that even though a Medicare Supplement insurance company cannot reject your enrollment for health reasons, the company is allowed to make you wait up to six months before covering your pre-existing conditions.
How long does Medicare Supplement open enrollment last?
How can enrollment periods affect my eligibility for Medicare Supplement plans? The best time to enroll in a Medicare Supplement plan is generally during your Medicare Supplement Open Enrollment Period —for most people, this period starts the month that you turn 65 and have Medicare Part B, and goes for six months.
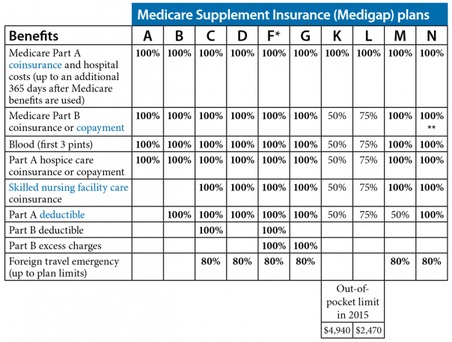
Does Medigap cover prescriptions?
Since Medigap plans don’t include prescription drug benefits, if you’re enrolled in Original Medicare and want help with prescription drug costs, you can get this coverage by enrolling in a stand-alone Medicare Prescription Drug Plan.
Does Medicare Supplement cover out-of-pocket expenses?
Medicare Supplement plans aren’t meant to provide stand-alone health coverage; these plans just help with certain out-of-pocket costs that Original Medicare doesn’t cover. If you’re under 65 and have Medicare because of disability, end-stage renal disease, or amyotrophic lateral sclerosis, your eligibility for Medicare Supplement coverage may ...
Qualification
- To be eligible for Medicare Part A and Part B, you must be a U.S. citizen or a permanent legal resident for at least five continuous years. You must also meet at least one of the following criteria for Medicare eligibility:
Results
- Be permanently disabled and receive disability benefits for at least two years: You automatically get Part A and Part B after you get disability benefits from Social Security for 24 months or certain disability benefits from the Railroad Retirement Board (RRB) for 24 months.
Diagnosis
- Have end-stage renal disease (ESRD) (permanent kidney failure that requires dialysis treatment or a kidney transplant): You need to sign up for Medicare, as your enrollment isnt automatic.
Causes
- Have Lou Gehrigs disease (Amyotrophic Lateral Sclerosis, or ALS): You automatically get Part A and Part B the month your disability benefits begin.
Cost
- Most individuals dont have to pay a premium for Medicare Part A if they or their spouse paid Medicare taxes while working for at least 10 years (or 40 quarters). If youre not eligible for premium-free Part A, you will have to pay a monthly premium of up to $437 in 2019. In addition, you must also pay the Part B premium each month. The standard premium is $135.50 in 2019.
Risks
- Also, keep in mind that individuals with a higher income may have to pay more for their Part B premium. Be aware that if you dont sign up for Medicare Part B when you first become eligible, you may have to pay a 10% penalty (added to your monthly premium) for each full 12-month period you could have had it but didnt sign up (some exceptions apply).
Benefits
- Medicare Part C (also called Medicare Advantage ) is an alternative way to your Medicare Part A and Part B benefits. Medicare Advantage plans are available through private insurers. To be eligible for Medicare Part C, you must already be enrolled in Medicare Part A and Part B, and you must reside within the service area of the Medicare Advantage plan you want. You can get more …
Prevention
- If you have end-stage renal disease (ESRD), you might not qualify for a Medicare Advantage plan in most cases. But theres one type of Medicare Advantage plan thats specifically meant for people with ESRD. Read about Medicare Special Needs Plans.
Access
- Medicare Part D covers prescription drugs and, like Medicare Part C, is available through private insurers that are approved by Medicare. To be eligible to enroll in a Medicare prescription drug plan (PDP), you must have Medicare Part A and/or Part B and you must live in the service area for the prescription drug plan in which you want to enroll. To be eligible to enroll in a Medicare Adva…