Physicians and other practitioners paid under the PFS bill for office/outpatient E/M visits using a set of CPT codes that distinguish visits based on level of complexity, site of service, and whether the patient is new or established. The three key components when selecting the appropriate code to bill are
Full Answer
How does Medicare pay for hospitals?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
What are the main features of traditional Medicare payment systems?
The main features of hospital, physician, outpatient, and skilled nursing facility payment systems (altogether accounting for almost three-quarters of spending in traditional Medicare) are described below: Inpatient hospitals (acute care): Medicare pays hospitals per beneficiary discharge, using the Inpatient Prospective Payment System.
What are the different parts of Medicare and how do they work?
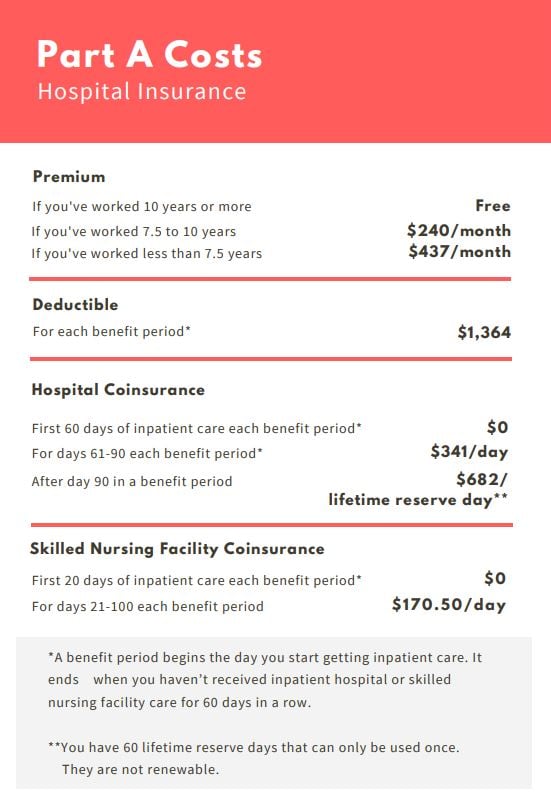
Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D. Now, while Medicare holders are responsible for paying their premium payments and deductibles, Medicare must pay the hospitals and other healthcare facilities to reimburse them for the medical care they provide.
Do nurse practitioners get paid less for billing Medicare?
In general, health professionals who are not physicians but bill Medicare independently (e.g., nurse practitioners) receive a 15 percent reduction in payment. Under current law, Medicare’s physician fee-schedule payments are subject to a formula, called the Sustainable Growth Rate (SGR) system, enacted in 1987 as a tool to control spending.
How does a physician bill Medicare?
Payment for Medicare-covered services is based on the Medicare Physicians' Fee Schedule, not the amount a provider chooses to bill for the service. Participating providers receive 100 percent of the Medicare Allowed Amount directly from Medicare.
Does Medicare pay doctors directly?
Rules for private contracts Medicare won't pay any amount for the services you get from this doctor or provider, even if it's a Medicare-covered service. You'll have to pay the full amount of whatever this provider charges you for the services you get.
How does Medicare decide what to pay?
Payment rates for these services are determined based on the relative, average costs of providing each to a Medicare patient, and then adjusted to account for other provider expenses, including malpractice insurance and office-based practice costs.
What percentage of the allowable fee does Medicare pay a doctor?
Under current law, when a patient sees a physician who is a “participating provider” and accepts assignment, as most do, Medicare pays 80 percent of the fee schedule amount and the patient is responsible for the remaining 20 percent.
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
How are physicians reimbursed for providing services to Medicare patients?
Medicare does not provide any reimbursement—either to the provider or the Medicare patient—for services provided by these providers under private contracts. Accordingly, Medicare patients are liable for the entire cost of any services they receive from physicians and practitioners who have opted out of Medicare.
How does Medicare work in simple terms?
Medicare is our country's health insurance program for people age 65 or older and younger people receiving Social Security disability benefits. The program helps with the cost of health care, but it doesn't cover all medical expenses or the cost of most long-term care.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
Why do doctors charge more than Medicare pays?
Why is this? A: It sounds as though your doctor has stopped participating with Medicare. This means that, while she still accepts patients with Medicare coverage, she no longer is accepting “assignment,” that is, the Medicare-approved amount.
What does Medicare pay per RVU?
On the downside, CMS set the 2022 conversion factor (i.e., the amount it pays per RVU) at $33.59, which is $1.30 less than the 2021 conversion factor. There was also mixed news on telehealth.
What is CMS physician fee schedule?
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
What is the SGR for Medicare?
Under current law, Medicare’s physician fee-schedule payments are subject to a formula, called the Sustainable Growth Rate (SGR) system, enacted in 1987 as a tool to control spending. For more than a decade this formula has called for cuts in physician payments, reaching as high as 24 percent.
Does Medicare have a fee for service?
Current payment systems in traditional Medicare have evolved over the last several decades, but have maintained a fee-for-service payment structure for most types of providers. In many cases, private insurers have modeled their payment systems on traditional Medicare, including those used for hospitals and physicians.
Does Medicare use prospective payment systems?
Medicare uses prospective payment systems for most of its providers in traditional Medicare. In general, these systems require that Medicare pre-determine a base payment rate for a given unit of service (e.g., a hospital stay, an episode of care, a particular service).
How many pages are there in the Medicare 2019 rule?
The proposed 1,473 page rule from the Centers for Medicare and Medicaid Services (you can read it here ), addresses two broad issues: 2019 payment rates for Medicare providers and more fundamental changes in the way the Trump Administration wants to compensate doctors, hospitals, and nursing homes.
What is the second option for ACO?
The second option, called the Merit-based Incentive Payment System (MIPS), does not require physicians to redesign their practices into ACO-like models, but offers modest financial rewards for achieving quality and outcome goals and imposes penalties for falling short. Most physicians participating in the new payment models have chosen MIPs.
Can small physician practices opt out of Medicare?
But small physician practices and even larger groups with few Medicare patients may opt out of the new payment system. CMS is also said it wants to experiment with excluding physicians in Medicare Advantage managed care plans from MIPs participation.
How much was Medicare reimbursement in 2015?
At the end of last year, it was reported by the American Hospital Association (AHA) that Medicaid and Medicare reimbursement in 2015 was less than the actual hospital costs for treating beneficiaries by $57.8 billion. That is billion with a “B”.
How much money do community hospitals provide?
Community hospitals provided more than $35.7 billion in uncompensated care to patients. The Centers for Medicare and Medicaid Services (CMS) does assist U.S. hospitals with additional funding. The Disproportionate Share Hospital payments help providers that treat large proportions of uninsured and Medicaid individuals.
Does Medicare cover medical expenses?
The ACA survey results showed that Medicaid and Medicare payments do not cover the amounts hospitals pay for personnel, technology, and other goods and services required to provide care to Medicare and Medicaid beneficiaries. This is critical in areas where the population is largely covered by Medicare and Medicaid.
Can hospitals participate in Medicare?
Despite low Medicaid and Medicare reimbursement rates and high uncompensated care costs, the AHA report pointed out that few hospitals can elect not to participate in federal healthcare programs. “Hospital participation in Medicare and Medicaid is voluntary,” noted the AHA.
When a patient uses Medicare as their primary insurance company, is the hospital required to choose appropriate and accurate diagnoses that
When a patient uses Medicare as their primary insurance company, the hospital is required to choose appropriate and accurate diagnoses that apply to the patient so that they can bill for the associated care.
What is Medicare insurance?
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
How long do you have to pay coinsurance for hospital?
As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed medically necessary. However, the remainder of the costs will be covered by your Medicare plan.
Does Medicare pay flat rate?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...