When submitting a paper corrected claim, follow these steps: • Submit a copy of the remittance advice with the correction clearly noted. • If necessary, attach requested documentation (e.g., nurses notes, pathology report), along with the copy of the remittance advice.
Full Answer
How to resubmit rejected claims?
To access this screen:
- Log on to FISS
- At the Main Menu screen, enter "01" and press <ENTER>
- At the Inquiry Menu screen, enter "12" and press <ENTER>
- At the Claim Summary Inquiry screen, type your National Provider Identifier (NPI) in the NPI field, the beneficiary's Medicare ID number in the HIC field, and FISS status/location R B9997 ...
Does Medicare accept corrected claim?
You can send a corrected claim by following the below steps to all the insurances except Medicare (Medicare does not accept corrected claims electronically). To submit a corrected claim to Medicare make the correction and resubmit as a regular claim (Claim Type is Default) and Medicare will process it.
What if Medicare denies my claim?
- Your bill will be sent directly to Medicare.
- The appeal must be filed within 120 days of receiving the Medicare Summary Notice (MSN) that shows that your claim was denied.
- If you disagree with a Medicare coverage decision in the MSN, you can appeal the decision.
What to do if Medicare denies your medical claim?
You can also take other actions to help you accomplish this:
- Reread your plan rules to ensure you are properly following them.
- Gather as much support as you can from providers or other key medical personnel to back up your claim.
- Fill out each form as carefully and exactly as possible. If necessary, ask another person to help you with your claim.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
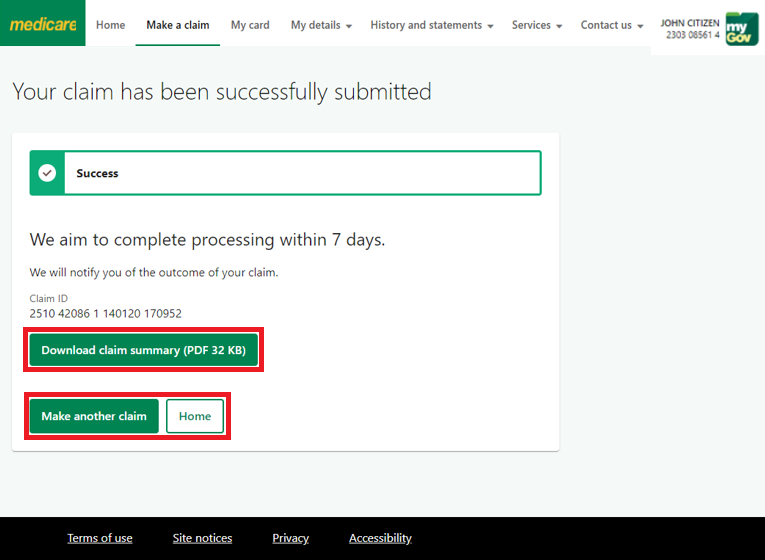
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
How long does it take to process a J15 claim?
Otherwise, you may contact the J15 Part A Provider Contact Center at (866) 590-6703 if the claim has not moved to a finalized location (XB9997) after 30 days (new claim) or 60 days (adjusted claim). The claim is missing information necessary to process the claim. The claim can be corrected or resubmitted.
When a claim is submitted to the Fiscal Intermediary Shared System (FISS), multiple editing processes are applied
When a claim is submitted to the Fiscal Intermediary Shared System (FISS), multiple editing processes are applied to identify possible errors. The chart below summarizes what happens to a claim that is subject to an edit and the appropriate process available to make claim corrections. Additional information about each claim correction process follows.
What is the redetermination process?
The redetermination process is the first level of appeal and applies to a claim or line item that receives a full or partial denial (identified as a claim in location DB9997 or a claim/line level reason code that begins with the number five or seven).
What is a redetermination in Medicare?
A redetermination is a written request, for a first level appeal, to the Medicare administrative contractor to review claim data when you are dissatisfied with the original claim determination. The redetermination is an independent process to re-evaluate the claim.
What happens if you request a redetermination?
If the request for a redetermination is not approved or unfavorable, you will receive a letter notifying you of the decision. Requesting a redetermination.
What is general inquiry?
A general inquiry is a written correspondence initiated by you that includes questions related to Medicare billing, processing or payments. There may be times that a redetermination cannot be accepted and the request will be forwarded to the general inquires department for a response to you.
How long does it take to get a redetermination from Novitas?
You have up to 120 days from the date of the initial determination of the claim to file a redetermination. We (Novitas) have 60 days upon the receipt of the request for redetermination to make a decision.
Can you file a redetermination over the phone?
Requests for redeterminations may not be filed over the telephone. All written redeterminations must contain the following items: The beneficiary name. The beneficiary Medicare number. The specific service (s) and/or item (s) for which the redetermination is being requested. The specific date (s) of service.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…