In 2016, individual EPs, EPs providing services at a CAH billing under method II, and PQRS group practices receiving a payment adjustment will be paid 2.0% less than the MPFS amount for that service. The 2016 payment adjustment is based on 2014 PQRS reporting.
What are the 2016 PQRS measures?
The 2016 PQRS measures address various aspects of care, such as prevention, chronic- and acute-care management, procedure -related care, resource utilization, and care coordination. EPs and PQRS group practices are not required to report on all of thePQRS measures and must select which measures they would like to report.
Which revenue codes will PQRS analyze for Medicare claims?
PQRS will analyze claims with 85X TOB , where “X” is any digit between 1 and 9, and physician supplier revenue codes (RCs) 045x, 096x, 097x and 098x , which will be paid based on the lesser of the submitted charges or the Medicare Physician Fee Schedule (MPFS). Note: The RCs and descriptions will change depending on the service location.
What are the individual PQRS measures related to diabetes and hypertension?
several individual PQRS measures related to diabetes, hypertension (HTN), and urinary incontinence, including the following: o Measure #1 (hemoglobin A1c poor control) with QDC 3045F + diabetes diagnosis E11.40 in form locator 67; o Measure #117 (diabetes - eye exam) with QDCs 2022F + diabetes diagnosis E11.40 in form locator 67; o
What is the role of PQRS in CMS Quality Strategy?
The vision for the CMS Quality Strategy is to optimize health outcomes by leading clinical quality improvement and health system transformation. PQRS plays a crucial role to facilitate physician participation in this process committed to quality improvement. Be a satisfactory reporter and avoid the 2018 PQRS negative payment adjustment.

What are the PQRS codes?
PQRS codes are used by CMS to measure the quality of care provided to Medicare Part B patients in the physician's office. CMS offers an incentive payment to practitioners for the satisfactory reporting of these codes to CMS.
What is PQRS and the Medicare EHR incentive Program?
The Physician Quality Reporting System (PQRS) is a voluntary reporting program for eligible physicians. PQRS encourages physicians to report data on quality measures for services furnished to Medicare Part B Fee-for-Service beneficiaries through a combination of incentive payments and payment adjustments.
Why is PQRS important?
Why is PQRS important to you? The program is voluntary, but for those physician practices and individual physicians that do not participate, they will be negatively impacted ECONOMICALLY. They will not be reimbursed at their traditional amounts, and it will impact their ability to keep and hire top physicians.
Are PQRS codes only for Medicare?
Is PQRS applicable to Medicare Advantage or to Medicaid patients? For most providers the answer is NO. Medicare claims-based submission was the only method available for 2007 Physician Quality Reporting Initiative (PQRI) so it was not feasible to include Medicaid only patients.
What is the difference between Pqrs and MIPS?
PQRS requires that participants report on at least 50% of the Medicare Part B Fee For Service patients who qualify for the chosen quality measures. MIPS requires that participants report on at least 50% of all patients who qualify for the chosen quality measures, regardless of payer.
When did MIPS replace Pqrs?
January 1, 2017A new quality program, the Merit-Based Incentive Payment System (MIPS), will replace PQRS on January 1, 2017.
What does PQRS measure?
The 2016 PQRS measures address various aspects of care, such as prevention, chronic- and acute-care management, procedure-related care, resource utilization, and care coordination.
How do physicians measure quality?
Typically, technical quality is measured using clinical information found in administrative databases, electronic health records, or medical charts, whereas interpersonal quality is measured using patient surveys.
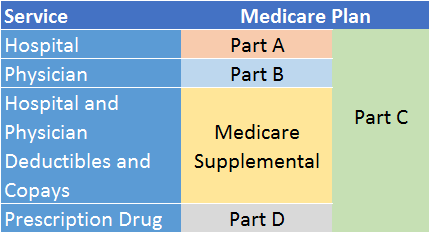
What is the meaningful use program?
'Meaningful Use' is the general term for the Center of Medicare and Medicaid's (CMS's) electronic health record (EHR) incentive programs that provide financial benefits to healthcare providers who use appropriate EHR technologies in meaningful ways; ways that benefit patients and providers alike.
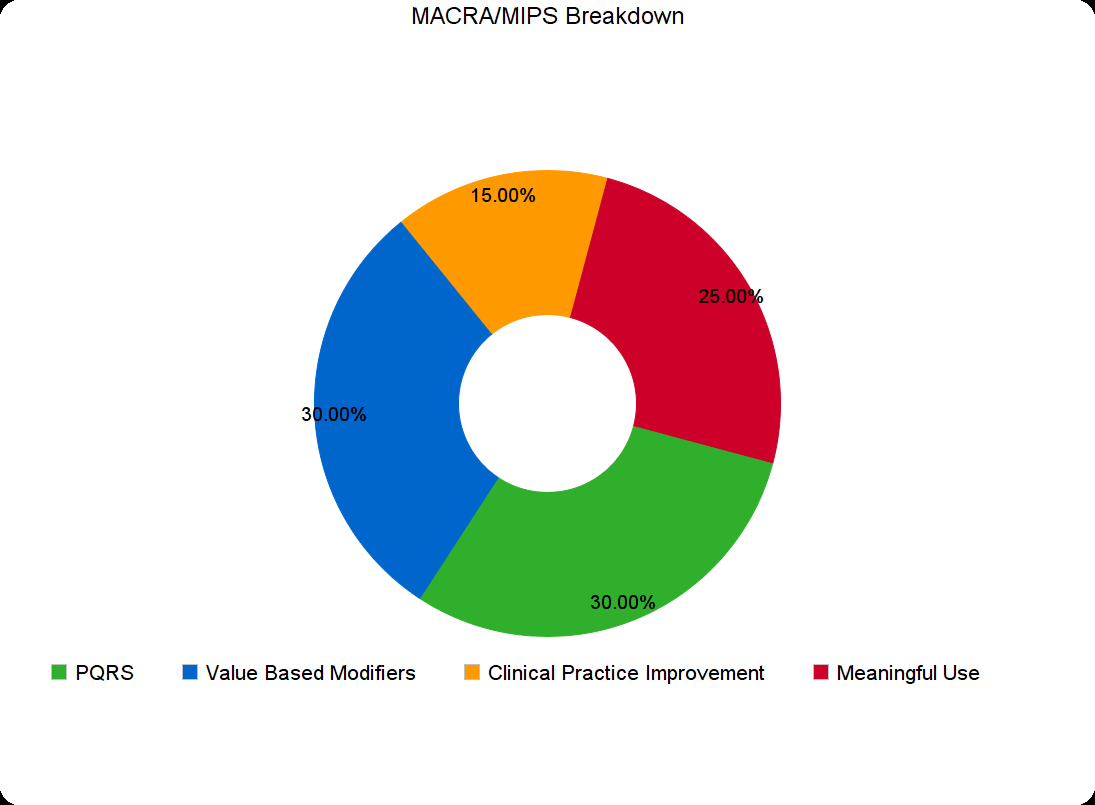
What are MIPS measures?
Traditional MIPS, established in the first year of the Quality Payment Program, is the original framework available to MIPS eligible clinicians for collecting and reporting data to MIPS. Your performance is measured across 4 areas – quality, improvement activities, Promoting Interoperability, and cost.
What is the full form of PQRS?
Acronym. Definition. PQRS. Physician Quality Reporting System (Medicare)
When did PQRS begin?
2006The Physician Quality Reporting System (PQRS), formerly known as the Physician Quality Reporting Initiative (PQRI), is a health care quality improvement incentive program initiated by the Centers for Medicare and Medicaid Services (CMS) in the United States in 2006.
What is PQRS in healthcare?
PQRS is a quality reporting program that uses negative payment adjustments to promote reporting of quality information by individual eligible professionals (EPs), EPs providing services at a Critical Access Hospital (CAH) billing under method II , and PQRS group practices participating in the group practice reporting option (GPRO). Those who do not satisfactorily report data on quality measures for covered Medicare Physician Fee Schedule (MPFS) services furnished to Medicare Part B beneficiaries (including Railroad Retirement Board, Medicare Secondary Payer, and Critical Access Hospitals [CAH] method II) or satisfactorily participate in a qualified clinical data registry (QCDR) will be subject to a negative payment adjustment under PQRS.
What is the CMS Physician Quality Reporting Programs Strategic Vision?
There are five statements which define the CMS Physician Quality Reporting Programs Strategic Vision (the “ Strategic Vision ”) for the future of such programs: CMS quality reporting programs are guided by input from patients, caregivers, and healthcare professionals.
When will the Medicare EHR incentive program end?
While PQRS, the Medicare EHR Incentive Program and the Value Modifier program will end in 2018, quality and performance-based reporting will remain a priority for CMS.
How many PQRS measures were there in 2016?
There are 13 individual PQRS measures in 2016 that are most likely to be used by psychologists depending upon the population they treat, the services they provide and the way in which they report. The individual measures are:
What is a PQRS measure group?
Measures groups are a subset of four or more PQRS measures that have a particular clinical condition or focus in common. All applicable measures within a group must be reported for each patient within the sample that meets the required criteria (such as age or gender). Eligible professionals can choose more than one reporting option (individual measures or measures groups), but can only earn a maximum of one incentive payment equal to 0.5 percent of their total estimated allowed Medicare charges.
What is PQRS in Medicare?
The Physician Quality Reporting System (PQRS) is a voluntary quality reporting program that applies a negative payment adjustment to promote the reporting of quality information by individual eligible professionals (EPs) and group practices . The program applies a negative payment adjustment to practices with eligible professionals (EPs), identified on claims by their individual National Provider Identifier (NPI) and Tax Identification Number (TIN), or PQRS group practices participating via the group practice reporting option (GPRO), referred to as PQRS group practices, who do not satisfactorily report data on quality measures for covered Medicare Physician Fee Schedule (MPFS) services furnished to Medicare Part B Fee-for-Service (FFS) beneficiaries (including Railroad Retirement Board and Medicare Secondary Payer). Those who report satisfactorily for the 2016 program year will avoid the 2018 PQRS negative payment adjustment.
What is a qualified registry?
qualified registry is an entity that collects clinical data from an EP or PQRS group practice and submits it to CMS on behalf of the participants. EPs and PQRS group practices participating should work directly with their chosen registry in order to submit data satisfactorily on the selected measures or measures groups (measures groups are only available to individual eligible professionals).
Who is required to report CAHPS?
Group practices with 100 or more will be required to report the CAHPS for PQRS measures through a CMS-Certified Survey Vendor in addition to satisfactorily reporting PQRS measures via qualified registry.
How many measures are there for Medicare?
Although extremely rare, the Centers for Medicare & Medicaid Services (CMS) recognize that a limited number of individual eligible professionals or group practices may not be able to identify 9 measures covering 3 domains that are applicable to their practice.
What is a GPRO?
A Group Practice Reporting Option (GPRO) that is greater than 100 eligible professionals is required to report CG-CAHPS. A GPRO that is less than 100 eligible professionals is not required to report CG-CAHPS. If CG-CAHPS is chosen to report, than it would be considered a cross-cutting measure for PQRS. 2016 PQRS M.
What is PQRS in Medicare?
The Physician Quality Reporting System (PQRS) is Medicare’s reporting program that asks eligible professionals (EPS), including psychologists, to submit data on specified quality measures to the Centers for Medicare and Medicaid Services (CMS). Reporting in PQRS consists of selecting measures that match your Medicare fee-for-service patients and identifying the services you provide to those patients. Medicare asks that you indicate whether or not the action described by the measures was taken through the use of a code (known as a “G” code) specific to each measure.
How many measures are required for EPs?
EPs must report on nine measures across three domains or report on 20 patients using a measures group. For EPs who have face-to-face encounters with patients one of the nine measures must be a cross-cutting measure.
What is a measure group?
Measures groups are a subset of four or more PQRS measures that have a particular clinical condition or focus in common. All applicable measures within a group must be reported for each patient within the sample that meets the required criteria (such as age or gender) G Codes are reported by the registry.
Is clinical depression screening documented?
Screening for clinical depression not documented, reason not given. G8432: Clinical depression screening not documented, reason not given. Screening for clinical depression documented as positive, follow-up plan not documented, reason not given.
Do measures groups need to be a qualified registry?
EPs reporting on a measures group must use a qualified registry as measures groups are not eligible for claims-based reporting. To successfully report the EP must perform the action described in the measure at least once. The EP’s reporting will not satisfy PQRS requirements if a measure has a zero performance rate.