What diagnosis codes are covered by Medicare?
covered code list. DME On the CMS-1500, if the Place of Service code is 31 (Nursing Facility Level B). S9123, S9124, Z5814, Z5816, Z5820, Z5999 Early and Periodic Screening, Diagnostic and Treatment (EPSDT) If services are part of Medicare non-covered treatment. J7999, J8499, S0257 End of Life Option Act (ELOA) Medicare denial not required.
What is a CBSA code for Medicare?
Medicare CBSA (Core-Based Statistical Areas) This product contains Medicare CBSA Codes, based on county, and assigned per ZIP Code for patient verification. If a ZIP Code crosses multiple counties, our file provides record for each occurrence. Medicare uses CBSA codes that are not identical to standard CBSA Codes.
What is Medicare place of service code?
Place of Service Codes is also known as POS codes in Medical Billing and are maintained by CMS –Centers for Medicare and Medicaid Services). This Place of Service codes is a 2 digit numeric codes which is used on the HCFA 1500 claim form while billing the medical claims to the health care insurance companies, denoting the place where the healthcare services was performed from the provider to ...
Does Medicare cover code 92133?
Claims for SCODI services (CPT codes 92133 and 92134) are payable under Medicare Part B in the following places of service: The global service is payable in the office (11), nursing facility (32- for Medicare patient not in a Part A stay) and independent clinic (49).
What does crossover with Medicare mean?
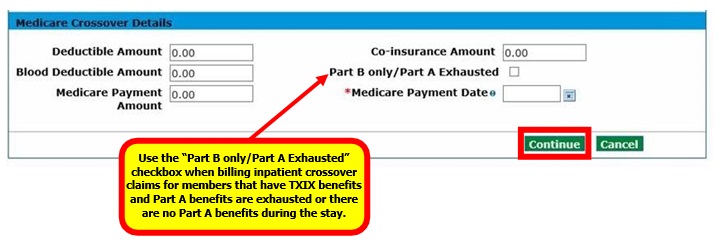
A crossover claim is a claim for a recipient who is eligible for both Medicare and Medicaid, where Medicare pays a portion of the claim, and Medicaid is billed for any remaining deductible and/or coinsurance.
When would you work a crossover claim?
In health insurance, a "crossover claim" occurs when a person eligible for Medicare and Medicaid receives health care services covered by both programs. The crossover claims process is designed to ensure the bill gets paid properly, and doesn't get paid twice.
Does Medicare automatically forward claims to secondary insurance?
If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
What is a crossover only application?
Crossover Only providers are those providers who are enrolled in Medicare, not enrolled in Medi-Cal, and provide services to dual-eligible beneficiaries. Dual-eligible beneficiaries are those beneficiaries who are eligible for coverage by Medicare (either Medicare Part A, Part B or both) and Medi-Cal.
Does Medicare crossover to AARP?
Things to remember: When Medicare does not crossover your claims to the AARP Medicare Supplement Plans, you will need to make sure this CO253 adjustment is applied before you electronically submit to AARP as a secondary payer.
How do I bill Medicare tertiary claims?
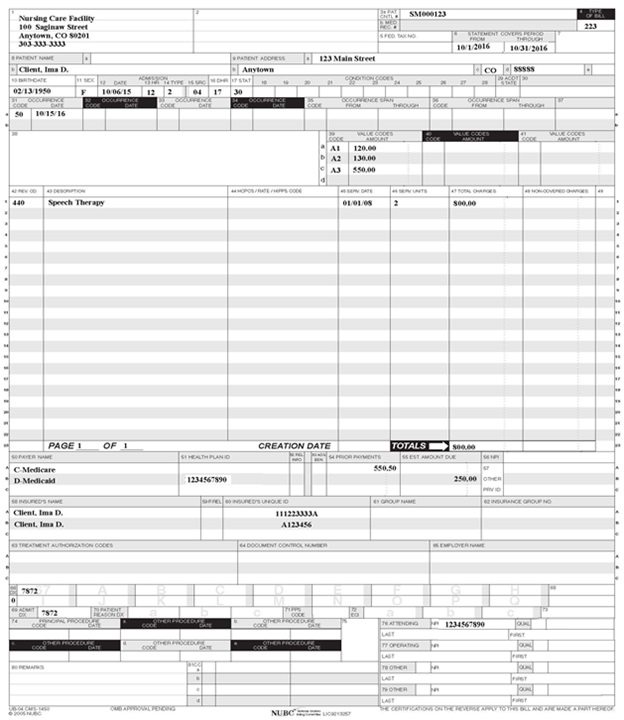
Tertiary Claims can be submitted through the Fiscal Intermediary Standard System (FISS) Direct Data Entry (DDE) or by paper utilizing the UB-04 form. At this time, tertiary claims cannot be submitted to Novitas electronically.
How do Medicare crossover claims work?
1. What is meant by the crossover payment? When Medicaid providers submit claims to Medicare for Medicare/Medicaid beneficiaries, Medicare will pay the claim, apply a deductible/coinsurance or co-pay amount and then automatically forward the claim to Medicaid.
What is crossover claim?
A crossover claim is a claim for a recipient who is eligible for both Medicare and Medi-Cal, where Medicare pays a portion of the claim and Medi-Cal is billed for any remaining deductible and/or coinsurance.
What determines if Medicare is primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
How do you create a crossover account?
Creating a Crossover Health account Access Crossover Health at: https://care.crossoverhealth.com/ Select “Sign up" to create your account. Preferred Email & Password: As a Crossover member, you will be able to receive communications from your doctor and Care Team via email. ... Enter your relevant information.More items...•
Where is crossover based?
Overview Suggest EditTypePrivateFounded2014HQAustin, TX, USWebsitecrossover.comEmployee Ratings3.3
What kind of company is crossover?
Crossover is a recruitment platform which specializes in 100% remote jobs. We connect talented professionals from around the globe with companies that are looking to hire the very best. Our 70+ client companies currently employ 4,000+ workers in 130+ countries.
What is a Medicare crossover claim?
Medicare crossover claims are claims that have been approved for payment by Medicare and sent to Medicaid for payment towards the Medicare deductible and coinsurance within Medicaid program limits.
How does Medicaid receive crossover claims?
How Medicaid Receives Crossover Claims. After providing a service to a dually-eligible recipient, the provider sends a claim to its Medicare carrier or intermediary. After Medicare processes the claim, it sends the provider an explanation of Medicare benefits. If Medicare has approved the claim, Medicaid can pay towards ...
Does Medicare pay for crossover?
Medicaid will not pay a crossover claim when it has been paid by Medicare in an amount that is the same or more than Medicaid’s rate for the specified service. Medicaid will not pay a crossover claim when it is for a service that is not covered by the Medicaid program.
Can Medicare pay for coinsurance?
If Medicare has approved the claim , Medicaid can pay towards the deductible and coinsurance according to Medicaid policy. Medicare crossover claims are submitted to the Medicaid fiscal agent by one of the following methods:
How to find if a Medicare claim is crossed over?
If a claim is crossed over, you will receive a message beneath the patient’s claim information on the Payment Register/Remittance Advice that indicates the claim was forwarded to the carrier.
How long does it take for Medicare to cross over to Blue Cross?
When a Medicare claim has crossed over, providers are to wait 30 calendar days from the Medicare remittance date before submitting a claim to Blue Cross and Blue Shield of Louisiana. Claims you submit to the Medicare intermediary will be crossed over to Blue Cross only after they have been processed by Medicare.
What is crossover process?
The crossover process allows providers to submit a single claim for individuals dually eligible for Medicare and Medicaid, or qualified Medicare beneficiaries eligible for Medicaid payment of coinsurance and deductible to a Medicare fiscal intermediary, and also have it processed for Medicaid reimbursement.
How long to wait to resubmit a Medicare claim in Louisiana?
What to do when the claim WAS NOT crossed over from Medicare For Louisiana claims that did not crossover automatically (except for Statutory Exclusions), the provider should wait 31 days from the date shown on the Medicare remittance to resubmit the claim.
What is a CIF for a crossover claim?
A CIF is used to initiate an adjustment or correction on a claim. The four ways to use a. CIF for a crossover claim are: • Reconsideration of a denied claim. • Trace a claim (direct billed claims only) • Adjustment for an overpayment or underpayment. • Adjustment related to a Medicare adjustment.
Is Michigan a secondary carrier for Medicare?
For example, if the member has a Medicare Supplement with Blue Cross and Blue Shield (BCBS) of Michigan, then BC BS of Michigan should be indicated as the secondary carrier, not Blue Cross and Blue Shield of Florida ( BCBSF).
Does MDHHS accept Medicare Part A?
MDHHS accepts Medicare Part A institutional claims (inpatient and outpatient) and Medicare Part B professional claims processed through the CMS Coordinator of Benefits Contractor, Group Health, Inc. (GHI). Claim adjudication will be based on the provider NPI number reported on the claim submitted to Medicare.
When will Medicare replace HIC?
Beginning April 1, 2018 , the Health Insurance Claim (HIC) number traditionally appearing on Medicare cards is being replaced by a non-Social Security Number based Medicare Beneficiary Identifier (MBI) number. Updated Medicare cards with MBIs will be phased into use through December 31, 2019. Therefore, the term HIC will be phased out of the Medi-Cal provider manuals, as appropriate. Removal of references to HIC does not preclude providers from processing transactions using HIC numbers. Providers can continue to process both HIC and MBI numbers, as appropriate, from April 1, 2018 through December 31, 2019. Providers should refer to the CMS website for detailed information.
What is Medicare Part A?
Medicare divides its services into Part A and Part B. Part A covers institutional services and Part B covers non-institutional services. Recipients may be covered for Part A only, Part B only or both.
What is Medi-Cal eligibility verification?
The Medi-Cal eligibility verification system indicates a recipient’s Medicare coverage when a provider submits a Medi-Cal eligibility inquiry. One of the following messages will be returned if a recipient is eligible for Medicare:
What is OHC in Village Health?
Medicare providers of services to dual-eligible VillageHealth Medicare Part C recipients should refer to the Other Health Coverage (OHC) section for instructions for requirements for billing coinsurance and/or deductible claims.
Is Medicare covered by Medicare?
Most medical supplies are not covered by Medicare and can be billed directly to Medi-Cal. However, the medical supplies listed in the Medical Supplies: Medicare-Covered Services section of the appropriate Part 2 manual are covered by Medicare and must be billed to Medicare prior to billing Medi-Cal.
Do you have to bill Medicare before you use Medi-Cal?
If a recipient has Medicare Part A coverage only, and a provider is billing for Part A covered services, the provider must bill Medicare prior to billing Medi- Cal. However, if billing for Part
Can you bill Medicare for coinsurance?
Providers who accept persons eligible for both Medicare and Medi-Cal as recipients cannot bill them for the Medicare deductible and coinsurance amounts. These amounts can be billed only to Medi-Cal. (Refer to Welfare and Institutions Code [W&I Code], Section 14019.4.) However, providers should bill recipients for any Medi-Cal Share of Cost (SOC). Note: Providers are strongly advised to wait until they receive the Medicare payment before collecting SOC to avoid collecting amounts greater than the Medicare deductible and/or coinsurance.