If Medicare refuses to pay a claim, you should call your doctor’s office to make sure they submitted the correct information. Sometimes, it’s just an oversight or human error that leads to a denial of coverage. If the claim was filed correctly but your insurance refuses to pay, you can file an appeal, also called a redetermination.
Full Answer
Why don't I get a bill from Medicare?
Most people don't get a bill from Medicare because they get these premiums deducted automatically from their Social Security (or Railroad Retirement Board) benefit.) Your bill pays for next month's coverage (and future months if you get the bill every 3 months).
Why do I still receive medical bills after my insurance pays?
If your healthcare provider is in-network with your insurance plan, then they’ll simply zero out the balance. If they’re out-of-network, however, whatever the insurance company does not pay for will be billed to you. This is why you may still receive medical bills after insurance pays its portion of your costs.
What does Medicare refuse to pay?
Medicare refuses to pay for a health care service, supply or prescription that you think you should be able to get. Medicare refuses to pay the bill for health care services or supplies or a prescription drug you already got. Medicare refuses to pay the amount you must pay for a drug.
Does Medicare pay more to some hospitals than others?
In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors. For example, hospitals that are teaching hospitals or those that treat a high proportion of low-income patients are eligible to receive increased payment.

What if Medicare does not pay?
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Does Medicare pay all your bills?
En español | Medicare covers some but not all of your health care costs. Depending on which plan you choose, you may have to share in the cost of your care by paying premiums, deductibles, copayments and coinsurance. The amount of some of these payments can change from year to year.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
How many days will Medicare pay for hospital stay?
90 daysMedicare covers a hospital stay of up to 90 days, though a person may still need to pay coinsurance during this time. While Medicare does help fund longer stays, it may take the extra time from an individual's reserve days. Medicare provides 60 lifetime reserve days.
What is the maximum out of pocket for Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
What percentage of medical bills Does Medicare pay?
80%In most instances, Medicare pays 80% of the approved amount of doctor bills; you or your medigap plan pay the remaining 20%, if your doctor accepts assignment of that amount as the full amount of your bill.
What is Medicare-approved amount?
The approved amount, also known as the Medicare-approved amount, is the fee that Medicare sets as how much a provider or supplier should be paid for a particular service or item. Original Medicare also calls this assignment. See also: Take Assignment, Participating Provider, and Non-Participating Provider.
Does Medicare only pay 80%?
Original Medicare only covers 80% of Part B services, which can include everything from preventive care to clinical research, ambulance services, durable medical equipment, surgical second opinions, mental health services and limited outpatient prescription drugs.
How long does it take Medicare to reimburse?
For clean claims that are submitted electronically, they are generally paid within 14 calendar days by Medicare. The processing time for clean paper claims is a bit longer, usually around 30 days.
How successful are Medicare appeals?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
How do I contact Medicare about a denied claim?
Call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. Visit Medicare.gov/forms-help-resources/medicare-forms for appeals forms. Call your State Health Insurance Assistance Program (SHIP) for free, personalized health insurance counseling, including help with appeals.
Does Medicare cover everything?
But like most forms of health insurance, the program won't cover everything. The services Medicare won't help pay for often come as a surprise and can leave people with hefty medical bills.
Does Medicare cover dental care?
Dental and Vision Care. Traditional Medicare does not cover the cost of routine dental care, including dental cleanings, oral exams, fillings and extractions. Eye glasses and contact lenses aren't covered either. Medicare will help pay for some services, however, as long as they are considered medically necessary.
Does Medicare Advantage cover dental?
Many Medicare Advantage plans, which are Medicare policies administered by private insurers, may offer benefits to help cover the cost of routine dental and vision care. But Lipschutz cautions that these extra benefits, while nice to have, tend to be quite limited.
Does Medicare pay for cataract surgery?
Medicare will help pay for some services, however, as long as they are considered medically necessary. For example, cataract surgery and one pair of glasses following the procedure are covered, although you must pay 20 percent of the cost, including a Part B deductible.
Does Medicare cover hearing aids?
The program will also pay for cochlear implants to repair damage to the inner ear. But Medicare doesn't cover routine hearing exams, hearing aids or exams for fitting hearing aids, which can be quite expensive when you're paying for them out of pocket.
Can you get Medicare out of area?
Out-of-Area Care. With traditional Medicare, you can get coverage for treatment if you're hospitalized or need to see a doctor while you're away from home inside the U.S. People covered by Medicare Advantage policies, however, generally need to see doctors within their plan's network for full coverage. If your plan is a preferred provider ...
Does Medicare cover drug addiction?
Opioid Dependence. Medicare helps pay for both inpatient and outpatient detox for alcoholism and drug addiction, although there are limits to the coverage. "The inpatient stay is covered during the most acute states when medical complications are more probable," Lind says.
When a patient uses Medicare as their primary insurance company, is the hospital required to choose appropriate and accurate diagnoses that
When a patient uses Medicare as their primary insurance company, the hospital is required to choose appropriate and accurate diagnoses that apply to the patient so that they can bill for the associated care.
How long do you have to pay coinsurance for hospital?
As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed medically necessary. However, the remainder of the costs will be covered by your Medicare plan.
What is Medicare insurance?
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
Does Medicare pay flat rate?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...
How much is 42.21 approved for Medicare?
You tell the billing department that Medicare approved 42.21 for the service them receiving the 80% of $33. You are paying the difference of 8.44 the balance Medicare says you owe. (or not if supplimental picks up then u say that). You tell them you are not paying more than Medicare approved.
Is 20% based on Medicare?
Explain that doctor is billing you more than approved amount. 20% is not based on the amount charged but the approved amount by Medicare. I think someone in the billing department has made a mistake. If the estate has no money, the bill can't be paid.
What happens if Medicare does not pay?
So if Medicare did not receive, or did not pay, a bill then your supplement company would never have any received the Medicare crossover request to pay their portion. Another tip as you investigate – make sure to record date/time that you called and who you speak with.
What happens after you call Medicare?
After you call Medicare itself and the provider’s office, you should have some answers to what happened or how it can be fixed. Sometimes, it’s as simple as a coding error on the claim. Other times, the provider’s office could have billed you while waiting for Medicare’s payment. Regardless, you should certainly pursue it ...
What to do if you get a bill that is incorrect?
If you get a bill that you think is incorrect, you should pursue investigating it.
Does Medicare give you information about your claims?
While Medica re will not give us information about your claims, due to HIPAA regulations, we can do a three-way phone call or guide you through the steps to finding a solution to the problem. Filed Under: Medicare News · Tagged: doctor's office billed medicare, medicare billing, medicare billing mistake, medicare code, medicare code mistake, ...
Does Medicare cover experimental medical bills?
Keep in mind that Medicare does not cover anything it considers experimental or not medically necessary.
Does Medicare Supplement pay when it does not?
That is a good starting point. From there, you know what to say when you call the doctor’s office.Keep in mind that Medicare Supplement plans (Medigap) pay when Medicare pays and do not pay when Medicare does not pay. So if Medicare did not receive, or did not pay, a bill then your supplement company would never have any received ...
What happens if you don't pay Medicare?
What happens when you don’t pay your Medicare premiums? A. Failing to pay your Medicare premiums puts you at risk of losing coverage, but that won’t happen without warning. Though Medicare Part A – which covers hospital care – is free for most enrollees, Parts B and D – which cover physician/outpatient/preventive care and prescription drugs, ...
What happens if you fail to make your Medicare payment?
Only once you fail to make your payment by the end of your grace period do you risk disenrollment from your plan. In some cases, you’ll be given the option to contact your plan administrator if you’re behind on payments due to an underlying financial difficulty.
How long does it take to pay Medicare premiums after disenrollment?
If your request is approved, you’ll have to pay your outstanding premiums within three months of disenrollment to resume coverage. If you’re disenrolled from Medicare Advantage, you’ll be automatically enrolled in Original Medicare. During this time, you may lose drug coverage.
How long do you have to pay Medicare Part B?
All told, you’ll have a three-month period to pay an initial Medicare Part B bill. If you don’t, you’ll receive a termination notice informing you that you no longer have coverage. Now if you manage to pay what you owe in premiums within 30 days of that termination notice, you’ll get to continue receiving coverage under Part B.
What happens if you miss a premium payment?
But if you opt to pay your premiums manually, you’ll need to make sure to stay on top of them. If you miss a payment, you’ll risk having your coverage dropped – but you’ll be warned of that possibility first.
When does Medicare start?
Keep track of your payments. Medicare eligibility begins at 65, whereas full retirement age for Social Security doesn’t start until 66, 67, or somewhere in between, depending on your year of birth.
When is Medicare Part B due?
Your Medicare Part B payments are due by the 25th of the month following the date of your initial bill. For example, if you get an initial bill on February 27, it will be due by March 25. If you don’t pay by that date, you’ll get a second bill from Medicare asking for that premium payment.
What happens when you visit a healthcare provider?
After you visit a healthcare provider that accepts your insurance, they’ll typically file a claim on your behalf. Your insurance company already has set rates that they’ll pay out for each type of service, and they’ll pay your provider that amount regardless of how much the provider has listed in their claim.
How much is medical claim denied?
Lauren Lau August 29th, 2019. It’s approximated that $3 trillion worth of medical claims are submitted every year to insurance companies, etc., with $262 billion worth of these claims denied. Approximately 65% of the denied medical claims are not resubmitted to the organization which denied the claim.
What is a misunderstanding between a healthcare provider and insurance company?
Another type of misunderstanding that can occur is one between your healthcare provider and your insurance company, something known in the medical billing industry as “bundling.”. Bundling is when a secondary procedure is considered part of a primary procedure.
What to do when your insurance doesn't pay for a service?
What to do when your health insurance doesn’t pay for a medical service. Insurance can be complicated, and medical billing can be even more difficult to understand. Most people would prefer to just go to the doctor’s office, have insurance take care of all the payments in the backend, and never think about the bills again. ...
What does it mean when your insurance provider is not in network?
If a provider accepts your insurance but is not in-network for your plan, it means they will bill your insurance company for the service and then charge the balance of what insurance won’t pay for directly to you. If you have a PPO plan, this typically means paying higher, out-of-network costs.
How to switch health insurance?
How can I switch insurance plans? 1 Marketplace/“Obamacare” plan. You can enroll in a Marketplace health insurance plan, also known as Obamacare or Affordable Care Act insurance. See plans and prices here. 2 Medicaid. You also may be eligible for Medicaid, depending on your income. You can see if you’re eligible and apply here. 3 COBRA. If you’ve been laid off recently, you usually have the option of COBRA, where you pay the full premium of the same insurance your employer purchased for you. COBRA is typically much more expensive than Marketplace insurance, but it allows you to continue the coverage you already had. Learn more about comparing COBRA with Obamacare health insurance. 4 Medicare. Once you turn 65, you’re eligible for Medicare. Call us to enroll at (855) 677-3060.
What is the reason for a doctor's visit?
Human error. It’s possible that your insurance company made an error in processing your claim, or perhaps they gave you misinformation that led you to make a doctor’s visit or undergo a treatment that isn’t fully covered. Or maybe your healthcare provider billed your visit incorrectly.
What happens if a hospital pays too little for work?
When a hospital or doctor thinks that a health insurer has reimbursed too little for the work or service that was done, federal and state laws will generally bar the medical providers from asking, and especially pressuring medical patients to pay the difference in the medical bill. Instead, the hospitals and doctors should be negotiating ...
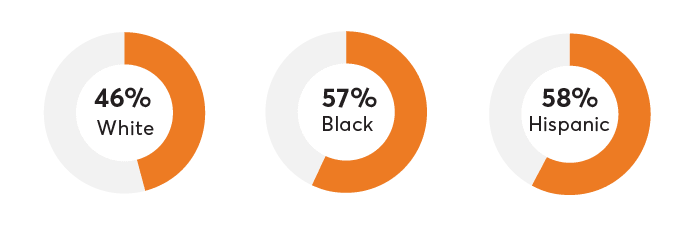
What percentage of consumers pay balance billing?
The group found that 56% of consumers paid the bills. Balance billing will most frequently occur with medical providers that participate in a managed-care network. It can occur from a doctor, dentist, or maybe even a pharmacy.
What is balance billing?
What exactly is balance billing? This is typically when an insurance plan will pay for less than what a hospital, doctor, or lab service wants to be paid for a medical bill. The healthcare provider than is demanding the balance of the bill directly from the patient.
Do you have to pay a bill to an out of network doctor?
Most state laws require medical providers to seek payment for a bill only from the insurer for any services covered by the plan. Many states will also protect insured patients from balance billing practices by all out-of-network doctors and hospitals in emergencies, since the patients usually do not control what doctor of hospital treats them in those situations.
Do you have to pay the balance between what insurance pays and what the medical cost?
So in other words, the patient is asked to pay the balance due between what insurance paid and what the medical care cost. The person does not need to pay this amount, and in some states this is being regulated or may even be illegal for the medical provider to demand payment.