Medicare does not cover an annual physical exam. Dunn, of Austin, Texas, was tripped up by Medicare’s confusing coverage rules. Federal law prohibits the health care program from paying for annual physicals, and patients who get them may be on the hook for the entire amount.
Full Answer
Will Medicare pay for a yearly physical exam?
Will Medicare pay for a yearly physical examination? En español | Medicare does not pay for the type of comprehensive exam that most people think of as a “physical.”
Does Medicare cover eye exams?
Original Medicare (Part A and Part B) usually doesn’t cover eye exams except in certain cases as described below. This summary of your Medicare benefits will help you understand your coverage.
Does Medicare cover the cost of a wellness exam?
The short answer is no, but it does cover a wellness exam. Here’s a question for you, “what’s the difference between a Medicare Annual Wellness visit versus an Annual Physical and which one is covered by Medicare?”
Does Medicare pay for Pap smear tests?
If you meet the eligibility criteria for the screening, the lab Pap smear test is free. The Pap smear test specimen collection, pelvic exam, and breast exam are also free if you get them through a doctor or other health-care provider that accepts assignment. For help figuring out your Medicare coverage options, feel free to ask me for help.

Does Medicare pay for yearly physicals?
As a rule, Medicare does not cover an annual physical. The exam and any tests your doctor orders are separate services, and you may have costs related to each depending on your Medicare plan.
Does Medicare cover yearly exams?
While Medicare does not cover annual physical exams, it does cover a single "initial preventive physical examination," followed by exams called "annual wellness visits.
What is the difference between a wellness visit and an annual physical?
An annual physical exam is more extensive than an AWV. It involves a physical exam by a doctor and includes bloodwork and other tests. The annual wellness visit will just include checking routine measurements such as height, weight, and blood pressure.
How often can Medicare wellness exams be done?
12 monthsfor longer than 12 months, you can get a yearly “Wellness” visit to develop or update your personalized plan to help prevent disease and disability, based on your current health and risk factors.
Does Medicare cover preventive visits?
Medicare pays for many preventive services to keep you healthy. Preventive services can find health problems early, when treatment works best, and can help keep you from getting certain diseases. Preventive services include exams, shots, lab tests, and screenings.
What does a full physical exam include?
A thorough physical examination covers head to toe and usually lasts about 30 minutes. It measures important vital signs -- temperature, blood pressure, and heart rate -- and evaluates your body using observation, palpitation, percussion, and auscultation.
Do Medicare wellness visits need to be 12 months apart?
Q - Do Medicare wellness visits need to be performed 365 days apart? A - No. A Medicare wellness visit may be performed in the same calendar month (but different year) as the previous Medicare wellness visit.
Can I refuse the Medicare Annual wellness visit?
The Medicare Annual Wellness Visit is not mandatory. While you may take advantage of these visits for free once per year, it's not a requirement to keep your Medicare benefits. There is no penalty if you choose not to go.
Is a well woman exam the same as an annual physical?
Well-woman exams include some of the same exams as a regular physical exam, like weight and blood pressure screenings and other important evaluations.
What is not included in a wellness visit?
Your insurance for your annual wellness visit does not cover any discussion, treatment or prescription of medications for chronic illnesses or conditions, such as high blood pressure, high cholesterol or diabetes.
How much does Medicare reimburse for annual wellness visit?
around $117Patients are eligible for this benefit every year after their Initial Annual Wellness Visit. The reimbursement is around $117.
Do Medicare wellness visits have to be 365 days apart?
A beneficiary who receives an AWV during a given month, for example, February 14, 2016, will be eligible for their next AWV on the first day of that month in the following year, February 1, 2017 in this example. A full 365 days is not required between Annual Wellness Visits.
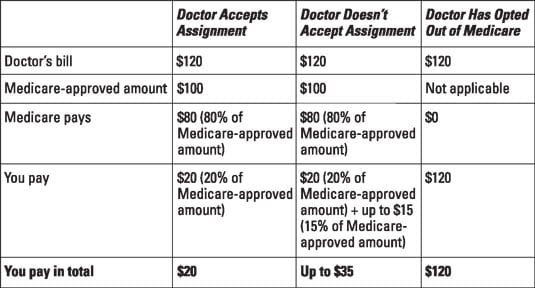
What does "assignment" mean in Medicare?
You’re enrolled in original Medicare (Part A and Part B) and you see a doctor who accepts “assignment” — meaning he or she accepts the Medicare-approved payment as full compensation. You’re enrolled in a Medicare Advantage (Part C) plan and see a doctor in the plan’s provider network.
Does Medicare cover wellness checkups?
But it does cover a one-time “Welcome to Medicare” checkup during your first year after enrolling in Part B and, later on, an annual wellness visit that is intended to keep track of your health. Initial visit: The “Welcome to Medicare” visit with your doctor aims to establish the state of your health when you enter the program and provide a plan ...
What is Medicare's Welcome to Medicare?
The main purpose of the “Welcome to Medicare” visit is for your health care provider to create a personalized prevention plan for your health care needs. Yearly Wellness Visit. Your Medicare Part B coverage includes preventive services, including an annual wellness visit.
Why is a health checkup important?
Your healthcare provider can use vital information gathered during a check-up to keep track of your current health condition, to evaluate your risk factors for future health problems, to create a care plan geared to keeping you healthy, and to inform you about healthy lifestyle choices.
Does Medicare cover annual health visits?
Medicare offers an initial health exam when you are first enrolled in Medicare coverage and annual health care visits. If you are enrolled in Medicare Part B coverage, you will be eligible for an initial “Welcome to Medicare” visit. After that, your Medicare coverage includes yearly “wellness” visits. Here are the details about what to expect ...
How long do you have to wait to get checked out of Medicare?
There is some good news, however. You actually do not have to wait until you’ve had Medicare Part B for 12 months before you can get checked out by your doctor. Medicare has a “Welcome to Medicare” preventive visit that you can take advantage of within the first 12 months of Part B coverage.
How long does a wellness visit last?
According to Medicare.gov, a “Wellness Visit” is covered once you’ve had Medicare Part B for longer than 12 months. If you have, you can get a “Wellness Visit” on an annual basis at no cost as long as the physician administering the exam accepts Medicare assignment. Also, there is NO Part B deductible or coinsurance applied.
Do you have to pay coinsurance for a wellness visit?
However, and this is a big “however,” the Part B deductible might apply and you could have to pay coinsurance if your health care provider performs additional services or tests during your Wellness Visit and if any additional tests or services are not covered under the Medicare preventive benefits.
Is a comprehensive physical exam covered by Medicare?
Comprehensive Physical Exam – Not paid for by Medicare Part B and typically not paid for by Medigap. Wellness Visit – 100% paid for by Medicare as long as your health care provider accepts assignment and does not go outside the services and tests covered under a Wellness Visit. Must have been enrolled in Medicare Part B for 12 months or more.
Does Medicare cover physicals?
Does Medicare cover a physical exam? The short answer is no, but it does cover a wellness exam. Here’s a question for you, “what’s the difference between a Medicare Annual Wellness visit versus an Annual Physical and which one is covered by Medicare?”
Is a physical covered by Medicare?
A physical is considered to be more comprehensive and is not covered by Medicare Part B like a Wellness Visit is. Here's what you can expect from your health care provider: Height, weight, and BMI measurement. Blood pressure measurement.
Is a wellness visit covered by Medicare?
As we mentioned earlier, the Wellness Visit is covered under Medicare Part B and your deductible will not apply. There is some good news, however.
How long does it take to get a Medicare physical?
Sometimes, companies call this a “ Welcome to Medicare ” physical. This exam is a one-time physical that a person must complete within 12 months of enrolling in Medicare Part B. Some of the tests that the IPPE includes are: This medical exam is free, as long as the doctor accepts assignment.
When a person schedules an annual wellness visit, should they contact Medicare?
When a person schedules an annual wellness visit, being specific about the type of appointment that they require may help them avoid any unwanted personal costs. If an individual is uncertain whether their plan will cover their appointment, they should contact Medicare in advance.
What is a routine physical exam?
tests to diagnose or treat a certain illness or disease. investigations into specific medical concerns. treatment and examination of injuries. Medicare will often consider anything other than these types of visits to be a routine physical examination, which they will not usually cover.
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
How often do you get a physical for Lou Gehrig's disease?
amyotrophic lateral sclerosis (also known as Lou Gehrig’s disease) A person is eligible for an initial physical examination within the first 12 months of Medicare enrollment. After that time, they are eligible for an annual wellness visit once every 12 months.
Does Medicare cover annual wellness visits?
Annual Wellness Visit (AWV) Medicare Part B covers yearly wellness visits, as it is the portion of Medicare that includes medical (usually nonhospital) services. The coverage of these wellness visits comes at no extra cost, as long as the medical provider accepts assignment.
What percentage of Medicare patients didn't get wellness visits in 2015?
That year, 18.8 percent of eligible beneficiaries received an annual wellness ...
What is Medicare's purpose?
When the Medicare program was established more than 50 years ago, its purpose was to cover the diagnosis and treatment of illness and injury in older people. Preventive services were generally not covered, and routine physical checkups were explicitly excluded, along with routine foot and dental care, eyeglasses and hearing aids. ...
What is a wellness visit for Medicare?
The focus of the Medicare wellness visit is on preventing disease and disability by coming up with a “personalized prevention plan” for future medical issues based on the beneficiary’s health and risk factors. At their first wellness visit, patients will often fill out a risk-assessment questionnaire and review their family ...
Does Medicare cover wellness visits?
Over the years, preventive services have gradually been added to the program, and the Affordable Care Act established coverage of the annual wellness visit. Medicare beneficiaries pay nothing as long as their doctor accepts Medicare. However, if a wellness visit veers beyond the bounds of the specific covered preventive services into diagnosis ...
Does Medicare cover physicals?
Medicare does not cover an annual physical exam. Dunn, of Austin, Texas, was tripped up by Medicare’s confusing coverage rules. Federal law prohibits the health care program from paying for annual physicals, and patients who get them may be on the hook for the entire amount. But beneficiaries pay nothing for an “annual wellness visit,” which ...
What are the benefits of Medicare Advantage?
Many Medicare Advantage plans include coverage for prescription drugs, as well as other benefits to help you manage your health-care costs, such as: 1 Benefits for routine vision care, including an annual eye exam and prescription eyewear 2 Coverage for routine hearing care 3 Optional dental care coverage for routine exams, cleanings, and even restorations and dentures 4 Benefits for wellness programs and discounted gym memberships
Is there a Part B for eye exams?
Except in the circumstances noted above, there is generally no Part B coverage for routine eye exams and vision checks. If you wear prescription eyewear or contact lenses, these costs are also not included in your Part B benefits, except in certain medical situations.
Does Medicare cover eye exams?
While Original Medicare doesn’t generally cover routine eye care, there are a few instances when your Part B coverage may help offset your eye exam costs: If you are considered to be at high risk for glaucoma (if you have diabetes, a family history of glaucoma, or are African American and over age 50, for example), ...
Does Medicare Advantage cover hospice?
Many Medicare Advantage plans include coverage for prescription drugs, as well as other benefits to help you manage your health-care costs, such as:
Does Medicare cover macular degeneration?
If your eye gets injured, Original Medicare may cover medically necessary diagnostic eye exams and treatment.
How often does Medicare cover mammograms?
If you are 40 years of age or older, Medicare will cover a screening mammogram every 12 months. If medically necessary, diagnostic mammograms may be covered more frequently. You will pay nothing for these lab tests, pelvic and breast exams as long as you go to a doctor who accepts assignment.
How much does Medicare pay for mammograms?
If your doctor orders a diagnostic mammogram, you will pay 20% of the Medicare-approved amount, and the Part B deductible applies. If you are enrolled in a Medicare Advantage plan, you will have at least the same Part A and Part B benefits as you would under Original Medicare, but many MA plans offer additional coverage.
How often do you get a Pap test?
Fewer than three negative Pap tests in the last seven years. Medicare Part B covers HPV (Human Papillomavirus) tests as part of a Pap test once every five years if you are between the ages of 30 and 65 without HPV symptoms.
What is gynecology in Medicare?
Gynecology is the branch of medicine that includes diseases and functions specific to women’s health, including the reproductive system. While many women on Medicare are over the age of 65 and past their reproductive years, others receive benefits under the age of 65 due to certain disabilities. Regardless of your age, access to preventive care, ...
Do you pay for mammograms if you accept assignment?
You will pay nothing for screening mammograms if your medical provider accepts assignment. When a doctor accepts assignment, they agree to be paid directly by Medicare, to accept the the payment amount approved by Medicare, and not to bill you for more than the Medicare deductible and coinsurance.
Does Medicare cover gynecology?
How Medicare Helps Cover Gynecological Care. Medicare’s Part B (Medical Insurance) coverage for a yearly Wellness Visit includes the components of a Well Woman Exam, which includes a clinical breast exam, Pap tests, and pelvic exam. These exams can be performed by your primary care physician or separately by a gynecologist.
How often is a Pap smear covered by Medicare?
All women with Medicare Part B are covered for these three screenings once every 24 months. You may be covered for a Pap smear once every 12 months if:
What is the difference between Medicare Advantage and Medicare Advantage?
The primary difference with Medicare Advantage is that you get Medicare benefits from a Medicare-approved private insurance company instead of directly through the government. Some Medicare Advantage plans include extra benefits such as prescription drug coverage.
What is the purpose of a Pap smear?
The primary goal of a Pap smear test is to screen for signs of cervical cancer. During the Pap smear test, your doctor uses a small spatula-shaped device to scrape a few cells from your cervix. The doctor then sends the cells to a laboratory to check for “pre-cancers” or cell abnormalities that can cause cervical cancer.
Can you stop a Pap smear test?
Women over 65 and women who have had a total hysterectomy (removal of the uterus and cervix) may be able to stop having Pap smear tests. If you’ve received an abnormal result, your doctor may recommend you get a Pap smear more frequently. Find affordable Medicare plans in your area. Find Plans.
Is a Pap smear free?
If you meet the eligibility criteria for the screening, the lab Pap smear test is free. The Pap smear test specimen collection, pelvic exam, and breast exam are also free if you get them through a doctor or other health-care provider that accepts assignment.